Mood swings and feelings of anxiety and sadness are common during both perimenopause and menopause.

Like most other symptoms, they can be associated with fluctuating hormone levels, specifically estrogen, progesterone, and serotonin. However, like anxiety and mood changes, depression during this time of life can also occur for reasons other than menopause. Hormonally speaking, the following is happening:
Estrogen & serotonin
The production of estrogen is correlated with the action of serotonin, a neurotransmitter that acts as our “happy hormone” by reducing anxiety and fostering feelings of well-being. So as estrogen levels fluctuate during the menopausal transition, serotonin pathways can be disrupted, which can affect mood.
Progesterone & GABA
Progesterone is the “calming hormone” that may also influence Gamma-Aminobutyric acid, or GABA for short. GABA is a neurotransmitter that produces a calming effect when it binds to its receptors. Progesterone potentiates (increases) the effects of GABA, so lower progesterone levels during perimenopause and menopause may result in less GABA-like activity, which the increases the chances of mood swings, anxiety, and sleeplessness.
Hormonal fluctuations can help explain why mood changes frequently pop up when we’re PMSing. After we ovulate but before we begin our period, we’re in what’s called the “luteal phase” where estrogen is high initially but then drops before your period starts (and remember, low estrogen can affect serotonin). This, along with progesterone fluctuations, can impact mood. Once we begin our period, estrogen levels rise, which causes our mood to stabilize.
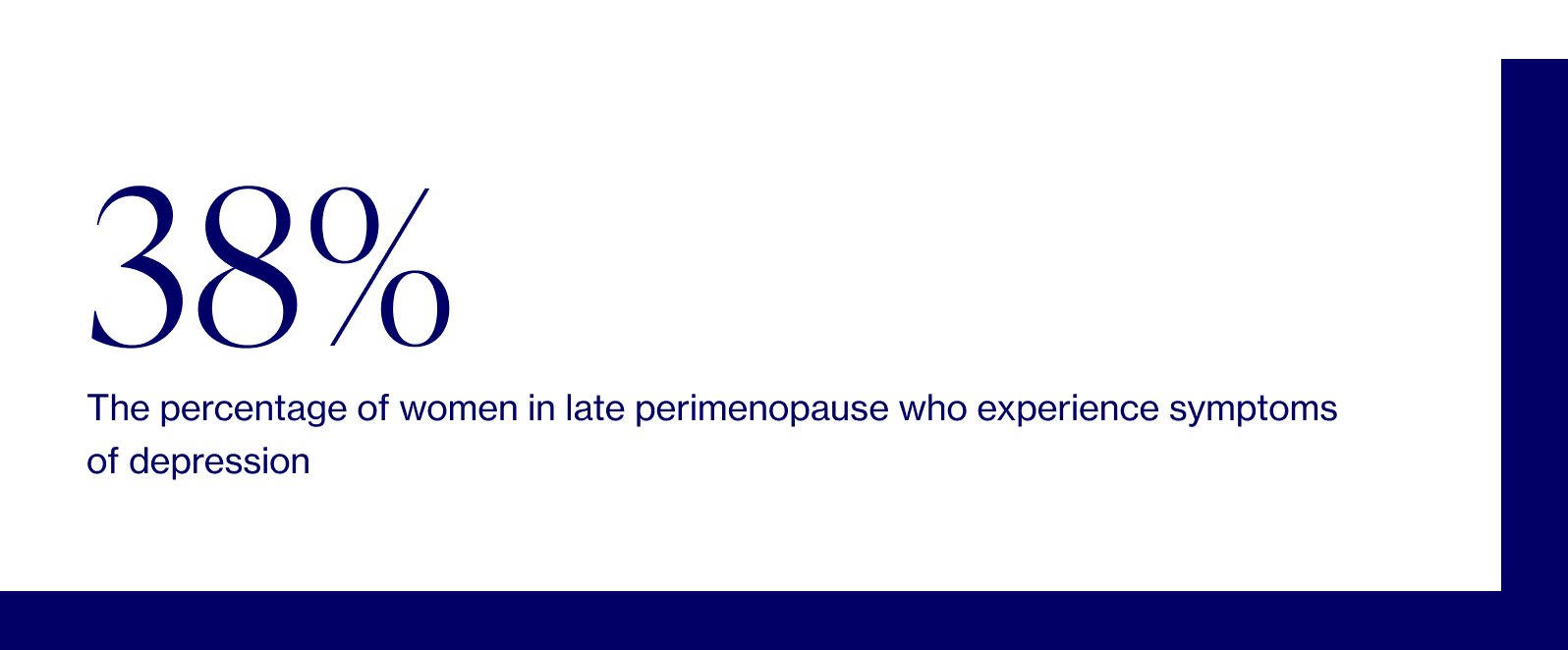
Women between the ages of 40 and 55 are more likely to report depressive symptoms than premenopausal or postmenopausal women, suggesting that the highest risk for new-onset depression is during the transition into menopause, not during postmenopause.
“There’s a new appreciation of the perimenopause — defined as the early and late menopause transition stages as well as the early postmenopause — as a window of vulnerability for the development of both depressive symptoms and major depressive episodes.” — Journal of Women’s Health
It’s important to note that there’s a difference between depressive symptoms and a depressive episode — symptoms may be sporadic and come and go over time, while episodes are when symptoms occur most of the day and nearly every day.
In addition to classic depressive symptoms, menopause also presents physical symptoms such as hot flashes/night sweats and sleep disturbances which can overlap and complicate the presentation of depression, leading some researchers to believe that there is a correlation (not causation) between the two.
Other menopausal symptoms often experienced simultaneously with depression include:
- Brain fog & difficulty concentrating
- Decreased energy
- Increased appetite
- Decreased libido (attributed to depression and/or vaginal dryness)
- Urinary incontinence (The science behind this potential association isn’t 100% understood but may be due to decreased serotonin levels in the central nervous system, which is correlated with symptoms of depression as well as increased urinary frequency/bladder contractions. Of course, urinary incontinence can be linked to multiple factors, including its well-established link to declining estrogen levels and physical changes of menopause.)
Mood swings and depression during this time can of course be independent of menopause (or compounded by it). In speaking with your provider about mood symptoms, s/he might ask a set of structured questions often used to screen for depression such as the PHQ9. These types of questionnaires can help identify depressive symptoms and, in turn, facilitate finding appropriate treatment.
Keep in mind that there are so many factors at play here that are difficult to discern: socioeconomic considerations, psychological, social, health, etc. Plus, let’s not forget that we’re dealing with our fair share of life stressors during this transition. Maybe we’re caring for children or aging parents, navigating career shifts, or struggling with our changing bodies. All of the above can adversely impact mood and should NOT be discounted as “par for the course.”
Severe symptoms like depression or anxiety that prevent you from functioning, disrupt relationships, and are associated with suicidal thoughts need medical attention and there is nothing shameful about it. In those situations, although we support integrative and holistic approaches, urgent medical care and even pharmacologic therapy may be appropriate first steps.
Dr. Anna Barbieri, MD
Pro tip #1
We know that women are more prone to mood changes around menopause; however, research shows that those who have undergone an oophorectomy (removal of ovaries) before natural menopause have an even higher probability of depression with more severe and longer-lasting symptoms. This underscores just how important mental health education is for all women. Taboos have NO place here.