Published on Sep 15, 2025
Last modified on Dec 22, 2025
Do I Need To Take a Vitamin D Supplement for Menopause?
7 min read
Vitamin D, or in science-speak “calciferol,” is a fat-soluble vitamin and essential nutrient for our overall health and well-being. While it is well-known for its role in supporting bone health, it also plays a large part in supporting our immune system function and muscle function and movement.
It can be found in food sources like…
- 🐟 Fatty fish
- 🥚Eggs
- 🍄 Mushrooms
- 🍊Vitamin D-fortified foods (breakfast cereal, dairy products, orange juice)
Menopause, vitamin D, and calcium
One of the biggest benefits of vitamin D is its role in calcium absorption, which is particularly essential during menopause. Why does it matter so much?
Well typically, estrogen slows down bone turnover and loss, but as estrogen levels decrease in perimenopause, we begin to lose some of that protection. In turn, we are at higher risk of developing osteoporosis, and consequently at higher risk of fractures and breaks. According to the Endocrine Society, up to 20% of bone loss happens after menopause, and we know that one in every two postmenopausal women will have osteoporosis and most will suffer a broken bone in their lifetime.
This is where the vitamin D and calcium duo comes in. Calcium provides the strength and hardness necessary to keep our bones healthy, and vitamin D makes sure that the calcium we consume is actually absorbed.
What else does vitamin D help with?
Outside of bone health, vitamin D is purported to help with several conditions and symptoms associated with the menopause transition:
1. Sexual health
Vitamin D may have a positive impact on sexual health symptoms associated with midlife including vaginal dryness and urinary tract infections.
2. Mood
More and more research suggests there is a correlation between vitamin D levels and mental health, and people at risk of developing depression may be more likely to be deficient.
3. Cardiovascular health
We do know that vitamin D deficiency is associated with higher risk of cardiovascular disease and type 2 diabetes, a particular concern for perimenopausal and postmenopausal women as they are already at increased risk of developing heart disease.
4. Immune function
Numerous reports indicate that low vitamin D levels are associated with increased risk of autoimmune disorders, such as rheumatoid arthritis and multiple sclerosis.
5. Hot flashes
Some research suggests that optimal vitamin D levels may be associated with less frequent hot flashes/night sweats.
Despite consensus on the relationship between vitamin D and these conditions, the jury is still out on vitamin D supplementation. For the large part, we don’t have enough data at this point to know exactly how much vitamin D would be necessary to provide protection, which is why it is not considered a first line of defense for treatment or prevention of these conditions. But that doesn’t mean it’s off the table…
READ MORE: Metabolic Health & Menopause: What’s The Connection?
What is the best form of vitamin D for menopause?
The three main ways to get vitamin D are through diet, supplements, or sun exposure. That said, it can be difficult to obtain adequate vitamin D levels through diet alone (unless you’re super keen on mackerel and sardines).
Around 5–15 minutes of midday sun exposure to uncovered arms and legs, most days of the week, is generally sufficient to maintain adequate vitamin D status in healthy adults during warmer spring, summer, and early fall. However, too much sun exposure can put us at increased skin cancer risk, so we don’t advise baking in the sun the entire day as part of a wellness regimen.
During the winter months, UVB (a type of ultraviolet light emitted by the sun) may not be intense enough for meaningful vitamin D production. For these reasons, vitamin D dietary supplements can be a useful tool…
Vitamin D supplements for perimenopause and menopause
Types of vitamin D supplements
Vitamin D supplements are available in two forms: vitamin D2 and vitamin D3. Clinicians often recommend vitamin D3 as it is more active and may be more effective.
How much vitamin D should I take for menopause?
The amount of supplemental vitamin D to take depends on several factors such as what you’re looking to address and whether or not you are getting enough from your diet. So, it’s important to work with your provider to land on an appropriate dosage (that goes for all supplements!). They may estimate your levels of vitamin D through a simple blood test.
Choosing a vitamin D supplement
When choosing a supplement, it’s important to remember that the FDA does not (we repeat, does NOT) verify that the supplements contain what they say they do or whether they’re contaminated with heavy metals, bacteria, or pesticides. With that in mind, it’s super important to keep an eye out for…
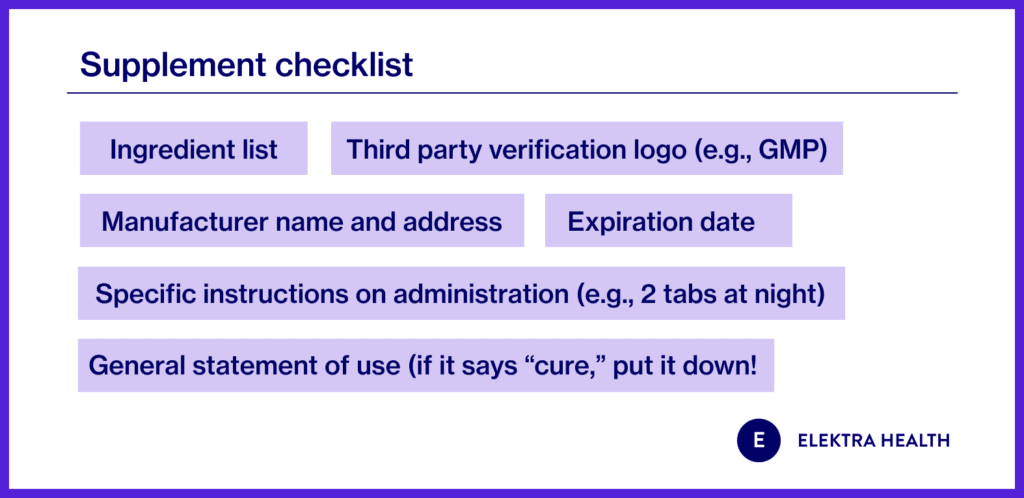
Read our full guide to supplements for menopause here >>
The bottom line
It’s well-established that vitamin D is important for bone density and health, and although more research is needed there is evidence to support that it also has an important role in sexual health, mood, immune function and heart disease prevention. During perimenopause and postmenopause as our risk of osteoporosis increases, it takes on an even more important role. For people who have difficulty getting enough vitamin D from diet alone, mindful supplementation can be a good option.
Frequently asked questions
Is there such a thing as too much vitamin D?
Technically, yes. Excessive vitamin D intake can cause buildup of calcium in the blood, which can pose serious health risks. That being said, toxicity is extremely rare, especially if you’re getting the vitamin from food sources or sun exposure. And for supplements, it would need to be an extremely high dose, well above what a clinician would prescribe.
Is there anything else I should be doing to support healthy bones?
Regardless of where in the transition you are, whether you’re a perimenopausal or postmenopausal woman, there are a few additional things you can do to supercharge your bone (and overall) health:
- Get enough protein: In the U.S., the RDA for protein is 0.36 grams per pound of body weight for adults.
- Get enough magnesium: An ideal balance is two parts calcium to one part magnesium. So if, for example, your multivitamin has 1,000 mg of calcium, it should have 500 mg of magnesium.
- Don’t forget about strength training: Strength training helps us maintain muscle mass (which we naturally lose), keeps our bones strong (which protects us from osteoporosis), and also helps with weight management and increasing our metabolic rate.
READ MORE: