You’ve likely heard the term menopause before. But what about perimenopause?
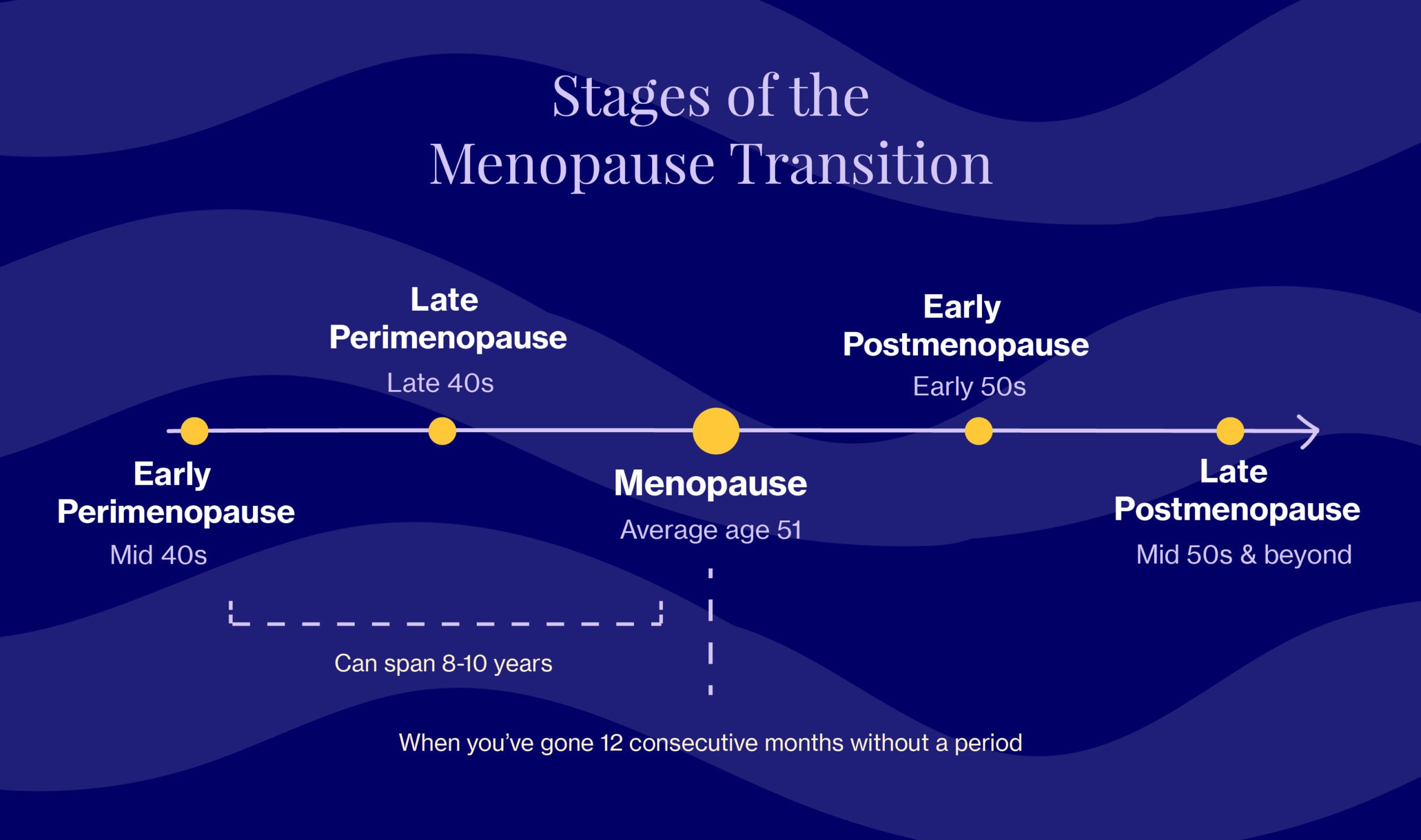
Most of us — even if we’re supported and informed — are thrown off when we hear this less-well-known word, which literally means “around menopause.” It’s used to describe the transition period between the onset of your first symptoms and the onset of menopause, which is technically marked by 12 consecutive months without a period (you can read more about that here). A doctor would say that you’re “in perimenopause” when cycles are irregular (i.e. varying by 7 days from your baseline, for example, a cycle of 33 days followed by a 26-day one) or when we skip cycles altogether.
If you’re thinking to yourself… WHAT?!…you’re not alone. Now’s as good a time as any to familiarize yourself with the start of this journey and begin building healthy habits for the years to come.
Knowing what’s happening in your body and why it’s happening is so powerful. When armed with this information, we can be proactive and preventive — and if we need support or help, we know where to go.
Never underestimate the advantage of preparation when navigating the menopause transition.
When, how & why
Perimenopause can be wildly unpredictable. Periods change dramatically, becoming heavier and more frequent, or they can go in the other direction. It’s generally a confusing time that catches a lot of us by surprise (so no, it’s not just you).
The transition in its entirety takes 8-10 years to move through, and while most of us will start in our mid-40s, some may begin years earlier. Perimenopause is often broken down into two general phases: early perimenopause (when periods can still be regular, which causes some confusion) and late perimenopause (marked by skipped and/or irregular periods — more aligned with what people typically think of when they hear perimenopause or menopause).
The takeaway? There’s no such thing as a one-size-fits-all experience. Hormonal changes, and the way symptoms show up, are anything BUT linear.
Like timing, perimenopause symptoms can vary, and each woman’s experience will be unique. We do know, however, that there may be certain racial and ethnic differences. One study in particular showed that African American women experience the worst vasomotor symptoms (hormone-related temperature dysfunction, e.g., hot flashes and night sweats), while Asian women reported the most mild.
Perimenopause symptoms: what to expect
It’s common to mistake the telltale signs of perimenopause — think hot flashes, night sweats, and mood swings — for those of menopause. But here’s a surprising fact: for many, these symptoms actually start to subside once we reach menopause, which means the worst may very well by over by this point (*cue the sigh of relief*).
Below are common symptoms that signal the beginning of perimenopause, all of which can be traced back to changing hormone levels. But remember, not everyone will experience these symptoms. Our goal here is to empower you with knowledge to manage the symptoms IF (key word) you do indeed experience them.
- Weight gain
- Worsening PMS with both emotional & physical changes (e.g., breast tenderness and heightened anxiety)
- Irregular periods, which is an umbrella term that can encompass short or skipped menstrual cycles and heavy bleeding (often one of the earliest symptoms)
Throughout the remainder of your journey, you may notice a number of the following perimenopausal symptoms (but not always, and not all at once): hot flashes and night sweats, irregular periods, difficulty sleeping, emotional changes (e.g., irritability, mood swings, and mild depression, especially before your period), difficulty with concentration and short-term memory, aka “brain fog,” vaginal dryness and/or discomfort during sex, and dry skin.
It sounds like a lot, we know, but we’ve broken down everything you need to know about every symptom — big and small — to empower you with science-based know-how and actionable solutions.
FAQ about perimenopause symptoms
Are the symptoms constant for the entire duration of menopause?!
It depends. Some symptoms come and go and others are more constant. What you can expect, however, is for symptoms to peak about 1-2 years prior to the onset of menopause due to an accelerated drop in estrogen levels.
How long will these symptoms last?
Typically five years — but remember, the perimenopausal experience isn’t one-size-fits-all for every woman again. Some may only experience a change in their period when nearing menopause, while others will experience it for upwards of 10 years.
Are these symptoms *always* due to perimenopause?
Not always, no. There are several common conditions, including thyroid abnormalities and even medication side effects that can cause similar symptoms, so be sure you are properly evaluated by your healthcare provider.
Is there a test for perimenopause?
Yes and no…it’s complicated. Doctors may order tests to check your hormone levels and thyroid function, but it’s imperfect at best since hormones fluctuate all. the. time. during perimenopause.
The low-down on hormones during perimenopause…what’s really happening?
Okay, so here’s what we know so far: hormonal fluctuations are to blame for the symptoms listed above. Great, but that doesn’t really help us. What does is diving into the science behind the symptoms which, in turn, helps us better cope with them. So stick with us…we’re breaking it all down below.
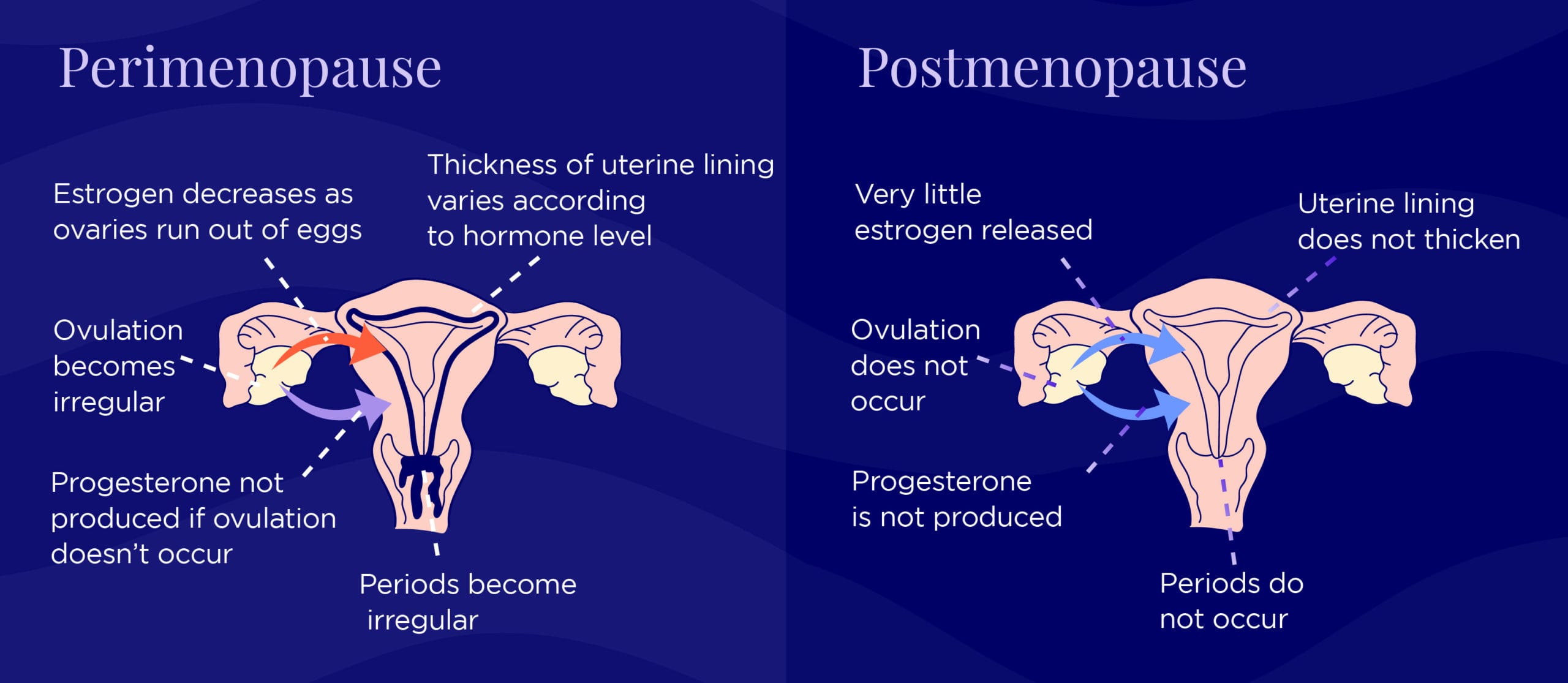
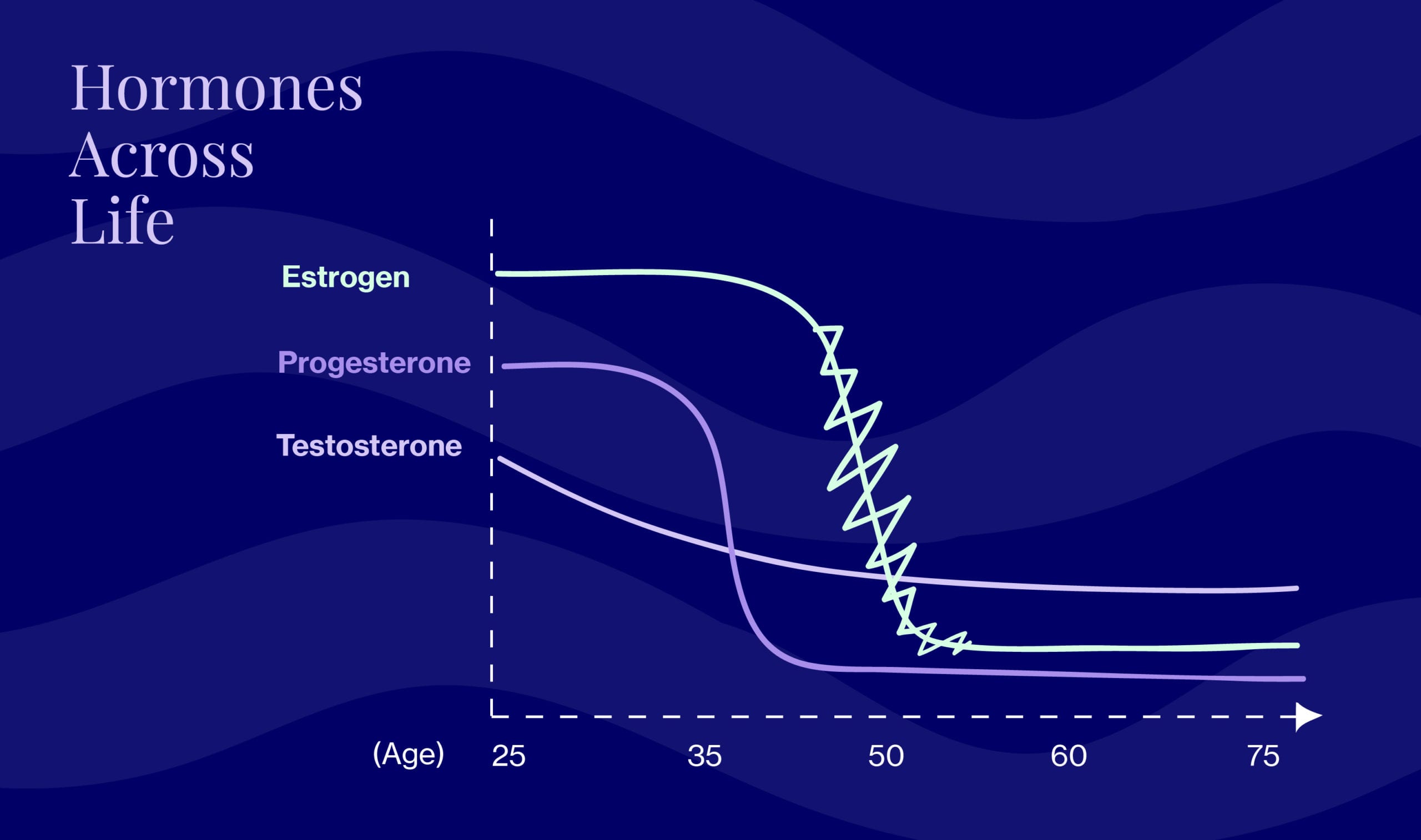
In our 20s and 30s (i.e. during premenopausal cycles), hormones enjoy a predictable ebb and flow. And in postmenopause, it’s low but steady. But the in-between perimenopausal period is marked by one long hormonal fluctuation, with levels of the two key female hormones (estrogen and progesterone) varying quite a bit. Progesterone starts to decline first, followed by estrogen, which fluctuates quite a bit as it does so. Testosterone is involved here as well, and slowly declines. So picture a rollercoaster – those are your hormones! And the rest of you is along for the ride. But those aren’t the only hormones that play a role.
Pre-menopause, FSH (follicle-stimulating hormone) and LH (luteinizing hormone) work together to produce a period. FSH causes eggs to mature in the ovaries, then LH triggers the egg’s release. During perimenopause, FSH levels fluctuate significantly, which means things get out of whack.
Wondering what hormones you should keep an eye on and/or test to determine (around) when you’ll hit menopause?
Estrogen
Menopause occurs when ovaries don’t produce enough estrogen for ovulation (which means no periods).
FSH
Although FSH was once considered the “test” for menopause, it’s not the most useful in perimenopause. Levels vary far too much to rely on it as a predictor of the last period.
AMH
Now, doctors look to AMH (the anti-mullerian hormone) to gauge the level of remaining egg cells — aka “ovarian reserve,” in doctor speak. AMH decreases with age until it becomes essentially undetectable around menopause. There are currently AMH tests in development, which could be used to assess whether a woman’s last period will occur in the next 18 months or so (via a blood test). Even though it’s possible to do an AMH test now, we don’t know that it can accurately ballpark your menopause “ETA”. So for the time being, AMH testing is not a typical part of the menopausal hormonal assessment.
Dr. Anna Barbieri, MD
Pro tip #1
For many, PMS kicks it up a notch during perimenopause, which often means exacerbated emotional symptoms, mood swings, and irritability. This is where mind/body practices like meditation can be helpful. Supplements can help, too, such as Seronal for emotional symptoms, and PMS Support for physical.
Dr. Anna Barbieri, MD
Pro tip #2
It’s natural to wonder when the menopause transition might happen. Until tests can provide more accurate and reliable answers, we recommend asking mom/aunts/sisters/[insert close female relative here] since timing of the menopausal transition is often genetic. We know this may not be an option for everyone — if that’s you, don’t sweat it. That’s what Elektra’s experts are here for!





