Published on Oct 28, 2025
Last modified on Dec 22, 2025
Can Menopause Affect Blood Sugar? What to Know
6 min read
When we consider the impact of menopause on our bodies, we tend to think of symptoms like hot flashes, poor sleep, mood swings, and vaginal dryness. But hormonal changes during this time of life can impact other systems in our body, including blood sugar management, which in turn impacts our risk of insulin resistance and type 2 diabetes.
We’re breaking down what you need to know about blood sugar changes in menopause and how to manage them.
How does menopause impact blood sugar?
Hormones play a large role in blood sugar regulation, specifically estrogen and progesterone. During perimenopause, we begin to see fluctuations in these hormone levels, which in addition to causing all sorts of symptoms, can also impact blood sugar levels.
Blood sugar and insulin resistance
Glucose is the primary source of energy for most of our body’s cells, and our bodies have several ways of keeping our blood glucose levels in a healthy range, including insulin. This hormone is responsible for regulating blood sugar levels and moving glucose from the bloodstream into our cells.
Sometimes though, our cells don’t respond as they should to insulin, which we call insulin resistance. When this happens, the pancreas starts to produce even more insulin to compensate. Insulin resistance can be caused by excess fat, low physical activity, poor diet, and some medications.
Over time, the pancreas may not be able to keep up and produce the amount of necessary insulin, which can lead to higher blood sugar levels, prediabetes, and eventually diabetes. The end result is that glucose just hangs out in the bloodstream, resulting in high blood sugar levels.
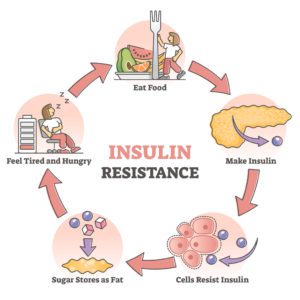
When we have insulin resistance, that increase in insulin can also lead to excess fat storage (especially abdominal fat), and because our cells aren’t getting the energy they need, we end up feeling hungry and tired. It’s a cascade of physiological events that gets stuck in repeat, leading to weight gain and other metabolic dysfunction.
Can menopause trigger diabetes?
While menopause doesn’t directly cause diabetes, it can contribute to risk factors for diabetes. This includes insulin resistance as we discussed above, in addition to the following:
1. Abdominal weight gain.
Accumulation of fat around the midsection, aka “meno belly,” is a common symptom associated with decreasing progesterone and estrogen levels around menopause. This increased abdominal fat can put us at a greater risk for health problems such as cardiovascular disease and type 2 diabetes.
It’s worth noting here the use of the word “accumulation,” which doesn’t necessarily mean the same thing as “extra weight.” Even if the number on the scale doesn’t change at all, insulin resistance and hormonal changes may lead to body fat redistribution from our hips and thighs to our waistline and abdomen.
2. Sleep disturbances.
Sleep problems such as difficulty falling asleep, nighttime waking, and sleep apnea are common symptoms of menopause owed to decreased estrogen, progesterone, serotonin, and melatonin, as well as increased cortisol (aka the stress hormone). Unfortunately, chronic insufficient sleep can put us at higher risk of type 2 diabetes.
Other risk factors for diabetes include family history, activity level, and early menopause — or menopause before the age of 45.
What does menopause look like for women who already have diabetes?
Premenopausal women who have been diagnosed with type 1 diabetes or type 2 diabetes are more likely to experience early menopause. This is important to pay attention to since it moves up our exposure to health risks associated with menopause such as weight gain, heart disease, and bone loss/osteoporosis.
If you are in your mid-30s and have type 1 or type 2 diabetes, it’s always a good idea to raise the question about what to expect during menopause with your healthcare provider, even if you’re not yet experiencing menopause symptoms.
How to keep blood sugar stable during menopause?
We know how overwhelming it can be to consider the vast potential implications of menopause on our health, such as high blood sugar, but the good news (finally!) is that there is plenty we can do on our own. Unsurprisingly, a lot of it comes down to lifestyle…
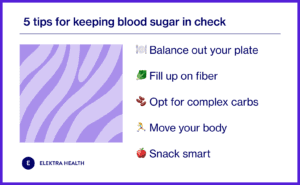
1. Balance out your plate.
Making sure your meals are balanced between vegetables, protein, and carbs is an easy way to make sure you’re getting all the important nutrients and keeping carbs in check to avoid post-meal glucose spikes. The American Diabetes Association recommends the following plate breakdown:
- Fill half your plate with non-starch vegetables
- Fill ¼ of your plate with a lean protein
- Fill ¼ of your plate with a carbohydrate
2. Fill up on fiber.
Fiber is something of a superhero micronutrient in that it supports digestion, helps with weight management, maintains gut health, and aids in blood sugar control. During the menopause transition, we should aim to get around 21 grams per day.
3. Opt for complex carbohydrates.
Say it with us: carbs are not the enemy. Complex carbohydrates like whole grains are an important part of a healthy diet. Unlike refined carbohydrates (think bagels and pizza), our body breaks them down slowly, which means they are more filling. They’re also less likely to cause those dramatic blood sugar spikes.
4. Move your body.
Integrating regular exercise is truly one of the best things you can do for your body during perimenopause and postmenopause. Not only does it help by improving insulin sensitivity and burning glucose, but also with weight and stress management.
5. Snack smart.
We get it, life gets busy and sometimes the easiest thing to reach for is a bag of chips or cookies. And while the occasional treat is okay, frequent consumption of processed foods can wreak havoc on our blood sugar levels.
The Bottom Line
As our ovaries slow down production of estrogen and progesterone during the midlife years, women often develop some degree of insulin resistance, which can result in higher blood sugar. Hormonal shifts can also lead to increased belly fat and sleep difficulties. In addition to their downstream effects on other aspects of our overall health and wellbeing, these physiological changes can contribute to our risk of type 2 diabetes. Fortunately, lifestyle changes can be a huge help and are in our control, such as prioritizing complex carbohydrates over refined and processed foods.
FAQs
Can menopause hormone therapy help?
Menopause hormone therapy, previously referred to as hormone replacement therapy or HRT, is the first line defense for treatment of hot flashes and night sweats in menopause. That said, it may also help lower fasting glucose levels as an added benefit. This refers to a measure of blood sugar after fasting overnight to see how your body regulates glucose.
Should I be using a continuous glucose monitor to track my blood sugar levels?
Continuous glucose monitors, or CGMs for short, are wearable devices that track your blood sugar levels in real time. They’re helpful for diabetics to make sure their bodies are processing glucose appropriately. However, they’re typically not necessary for nondiabetics and for that reason also aren’t likely to be covered by insurance.
Can supplements help with blood sugar control?
There are lots of supplements and blends which are marketed for weight loss. Unfortunately, if they sound too good to be true, they likely are. Some contain excessive amounts of caffeine, for example, which could cause side effects. If you consider any specific weight loss supplements, we recommend that you discuss with your doctor.
Is there a link between diabetes and breast cancer?
Women with type 2 diabetes are at a slightly increased risk of developing breast cancer, with the condition impacting nearly ⅓ of breast cancer patients. The mechanics of this relationship aren’t necessarily cut and dry, but evidence points to obesity and insulin resistance, both of which are comorbidities or diabetes and risk factors for breast cancer.
READ MORE: