We’re all about equipping you with the know-how to understand your symptoms, and we especially emphasize the specific, tangible ways to manage them. Our goal is to empower YOU to take charge of your menopause journey, starting today.
A quick note about product recommendations…Elektra Health is not paid to feature any products. We just like them and think you might too, though we can’t guarantee any results.
Many lifestyle changes have been evaluated for their effect on PMS and PMDD symptoms, including exercise, nutritional modifications, mind-body practices, and acupuncture. However, with so many avenues to take, it can be hard to know where to start. That’s why it’s necessary to have a healthcare provider (or Elektra!) who can work with you to chart the best way forward.
Lifestyle
Nutrition & Diet
The Standard American Diet — which tends to be high in carbs, fat, sugar, and salt — is directly correlated with increased PMS and PMDD symptoms. That’s why, when it comes to nutritional interventions for mood changes, we want to move towards low-glycemic-index diets that won’t dramatically spike our blood sugar (which in turn affects mood). Here are some helpful tips:
- Limit or eliminate sugar-sweetened beverages and alcohol
- Kick processed foods to the curb
- Incorporate more green leafy vegetables, nuts, fatty fish (e.g., salmon and sardines), berries, and dairy (if tolerated)
It’s also important to incorporate diuretic foods that decrease bloating and water retention, such as parsley, tomatoes, tomatoes, onions, garlic, asparagus, and watermelon…but not coffee. For more information on nutrition during menopause, check out Elektra’s guide.
Holistic Practices
Before having any conversations around hormonal interventions for mood changes, lifestyle factors such as stress and sleep must be addressed — which is easier said than done when everything and everyone seems to be competing for your attention.
Here’s what Elektra’s founding physician, Dr. Anna Barbierei, MD recommends:
To reduce stress:
Get out in nature
Routine, frequent exposure to the great outdoors has been shown to reduce anxiety and depression while improving an overall sense of well-being. Don’t underestimate Mother Nature!
Cultivate a meditation practice
Over time, you’ll condition yourself to be more present while letting thoughts come and go. We recommend guided meditations on apps such as Headspace, Insight Timer, and Calm.
Cultivate a gratitude and/or journaling practice
Studies have linked both practices to decreased anxiety, and they can also help improve general feelings of well-being and facilitate mindfulness. Here are some great tips on how to start a gratitude practice.
Prioritize downtime with family & friends
While we may be conditioned with a “go-go-go” mentality, it’s important to step back and prioritize rest and downtime with loved ones (pencil it into your calendar!). After all, human beings are social creatures, and we derive comfort from connection.
Don’t forget about “me” time
Call it what you want — self care, alone time, R&R — but you deserve it. There’s nothing “selfish” about taking time for yourself, especially when it supports your mental health and overall wellness. Think of it as putting your mask on first in an airplane, so you can be better equipped to help others.
Prioritize sleep
To improve sleep, we usually need to pull a few different levers – there is usually no single solution. It’s all about sleep hygiene (completely weird term, we know). Lifestyle factors like exercise and diet, routines and schedules, and calming activities are all part of it, and sometimes, select supplements can play an important role too. But doing what needs to be done to improve sleep is critical. For a deeper dive into how to improve sleep, check out Elektra’s guide to sleep issues.
There is no managing mood swings if you’re sleep-deprived!
Exercise
Scientists have found that regular movement decreases overall levels of tension, elevates and stabilizes our mood, improves sleep, boosts self-esteem, and eases PMS symptoms. Not too shabby, right? To reduce anxiety, we recommend a mix of aerobic cardio (preferably high-intensity interval training) several times per week due to its positive effect on mood and depression, strength training, and yoga or qigong, an ancient practice of coordinated body movement, meditation and breathing.
Supplements & Over-the-Counter Solutions
Supplements and over-the-counter solutions may be effective in supporting your mood symptoms…if you choose wisely. We recommend consulting with your healthcare provider first to ensure you’re using something with optimal efficacy and safety (i.e. backed by clinical research) or consulting with Elektra’s providers. Here’s a quick primer from our team on how to go about selecting high-quality supplements.
Many supplements and herbs have been evaluated for treatment of PMS and PMDD, while others are designed to foster a sense of calm by helping to reduce levels of everyday stress and promote high-quality sleep.
Swedish Flower Pollen
Swedish flower pollen, which is marketed as the product Serenol, is an extract made from the pollen and pistils of a certain family of grasses. When taken every day, it helps provide hormone-free relief from emotional symptoms such as mood swings, irritability, and uneasiness. (Note: Serenol contains royal jelly, which is weakly estrogenic, so it’s not recommended for women with hormone-positive breast cancer.)
Vitex (aka Chasteberry)
The hormone-balance properties of Vitex have been found to help relieve symptoms of perimenopause, including PMS-related mood changes
Ginger
Studies have shown ginger to be effective in reducing the severity of both mood and physical PMS symptoms.
There are other supplements that may help with mood regulation, like magnesium, GABA, St. John’s. Wort, and kava kava, but we encourage discussion with a trained provider (like Elektra!) to ensure their appropriateness and lack of interaction with other supplements or medications.
Prescription
Hormonal
We tend to focus on sleep, nutrition, and stress management — all of which can have an incredibly powerful impact on symptoms — before turning to hormonal treatments for menopause-related mood changes. If you do opt for hormonal treatment (for example, low-dose birth control for severe PMS and PMDD in early perimenopause), it should be coupled with mind-body interventions. In other words, nothing should exist in a silo, especially for something as complex as our mood.
Data are mixed about whether HRT helps with mood issues like anxiety, which can contribute to mood changes, with smaller studies showing conflicting results or no effect. However, it is reasonable to consider hormonal treatment, especially if one has other symptoms that we know can be helped by HRT (like hot flashes) to help with mood fluctuations. Refer to our complete guide for a full run-down on hormone replacement therapy (HRT).
Non-Hormonal
SSRIs and SNRIs remain the first line of pharmacologic defense for mood changes, as well as anxiety and depression in perimenopausal women who are unable or not interested in hormonal therapies, and can also be considered for mood changes.
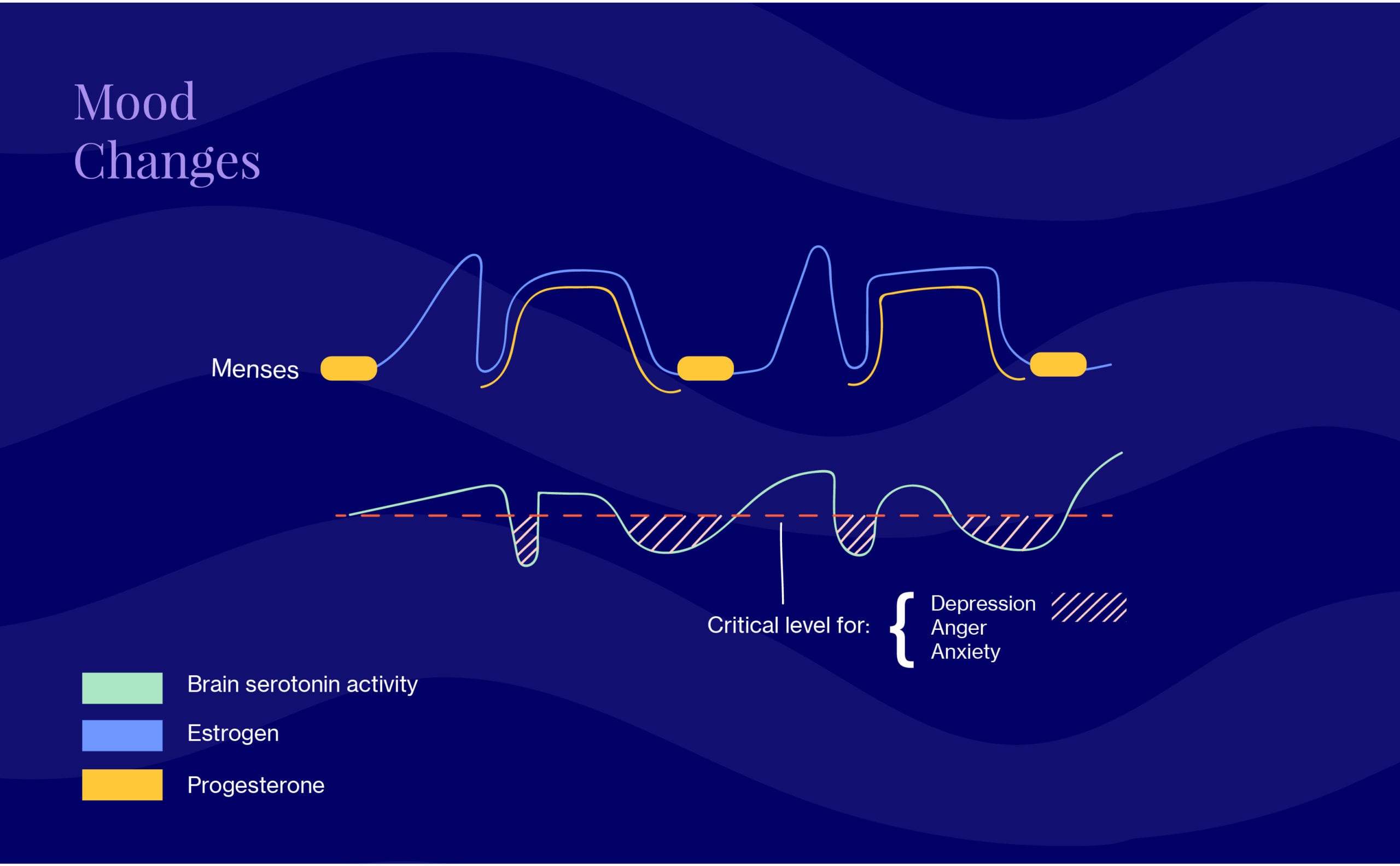
SSRIs are selective serotonin reuptake inhibitors and SNRIs are serotonin and norepinephrine reuptake inhibitors — total tongue-twisters! These neurotransmitters are antidepressants that work by regulating serotonin (the “happy hormone” that controls mood) and norepinephrine (plays a key role in the body’s “fight-or-flight” response to stress). Numerous trials have demonstrated their safety and efficacy for severe mood-related PMS and PMDD symptoms, although it should be noted that common side effects include weight gain and low libido.
Common SSRIs include fluoxetine/Prozan and sertralin/Zoloft. Other examples are:
- Escitalopram/Lexapro: associated with less weight gain and sexual side effects (i.e. low libido) than others
- Venlafaxine/Effexor: associated with higher risk of withdrawal symptoms, so proper weaning is important and should be done under the guidance of your provider
If you’re experiencing an emergency and need immediate help, call 911 or go to the nearest emergency room.
Suicide Prevention Lifeline
+ 1-800-273-8255
Crisis Text Line
Text HOME to 741741
We’re always keeping an eye out on emerging research and the latest clinical studies. Subscribe to our weekly Elektra Digest for the latest, science-based info direct to your inbox. Something work well for you that’s not listed here? We want to hear it! Shoot us a note at [email protected]. (We’re human, promise.)
Pro tip #2
On the hunt for recipes that are delicious but won’t spike your blood sugar (and mess with your mood)? Allrecipes has a dedicated collection of over 1,000 low glycemic impact meals — with associated videos! — that are chock-full of fiber and protein. Braised balsamic chicken, anyone? What about miso soup?
Pro tip #3
It’s sometimes hard to know if or how to seek medical advice for menopause symptoms like mood swings. As a good rule of thumb, if changes to your mood around this transition make it difficult to be present and participate in everyday activities, it’s worth talking to your doctor or Elektra to discuss how you feel and what your options might be.
Disclaimer: This information is for general educational purposes, and should not be used as a substitute for medical advice, diagnosis or treatment of any health condition or problem.
As with anything you put into your body, taking dietary supplements can also involve health risks. You should consult a medical professional before taking supplements and inform your doctor about any supplements, as well as any medications you already take, since there may be interactions.
Helpful? Share the wealth!
Share with a friend who deserves evidence-based expertise &
solutions.