Published on Feb 13, 2026
Last modified on Feb 13, 2026
Elektra’s Take: Testosterone for Menopause
7 min read
Testosterone has been commanding the room, aka the algorithm, for some time now. If you’ve been noticing some mixed messages or extreme claims from wellness influencers (e.g. “every midlife woman should be taking testosterone”), you’re not alone. We’re seeing the same thing — and yes, it’s confusing. The reality is, this topic is nuanced, and a simple yes/no, good/bad won’t serve anyone here. With that let’s dig into whether or not it’s safe (it’s complicated), what “benefits” are actually supported by evidence (and which ones aren’t), and why it IS such a big deal that we get this conversation right.
The role of testosterone in the body
Testosterone belongs to a group of sex hormones called androgens, and is produced in men and women. While long considered a “male hormone,” it also plays an important role in female sexual function. In women, testosterone is produced in the ovaries and adrenal glands, with peak production in our late 20s.
New research has given us greater insight into the course of testosterone levels in women across ages. After that late-20s peak, testosterone levels decline until the late 50s, when the hormone can “bounce” back, though not to previous levels. (Removal of the ovaries, or an oophorectomy, can also contribute to a more abrupt decline).
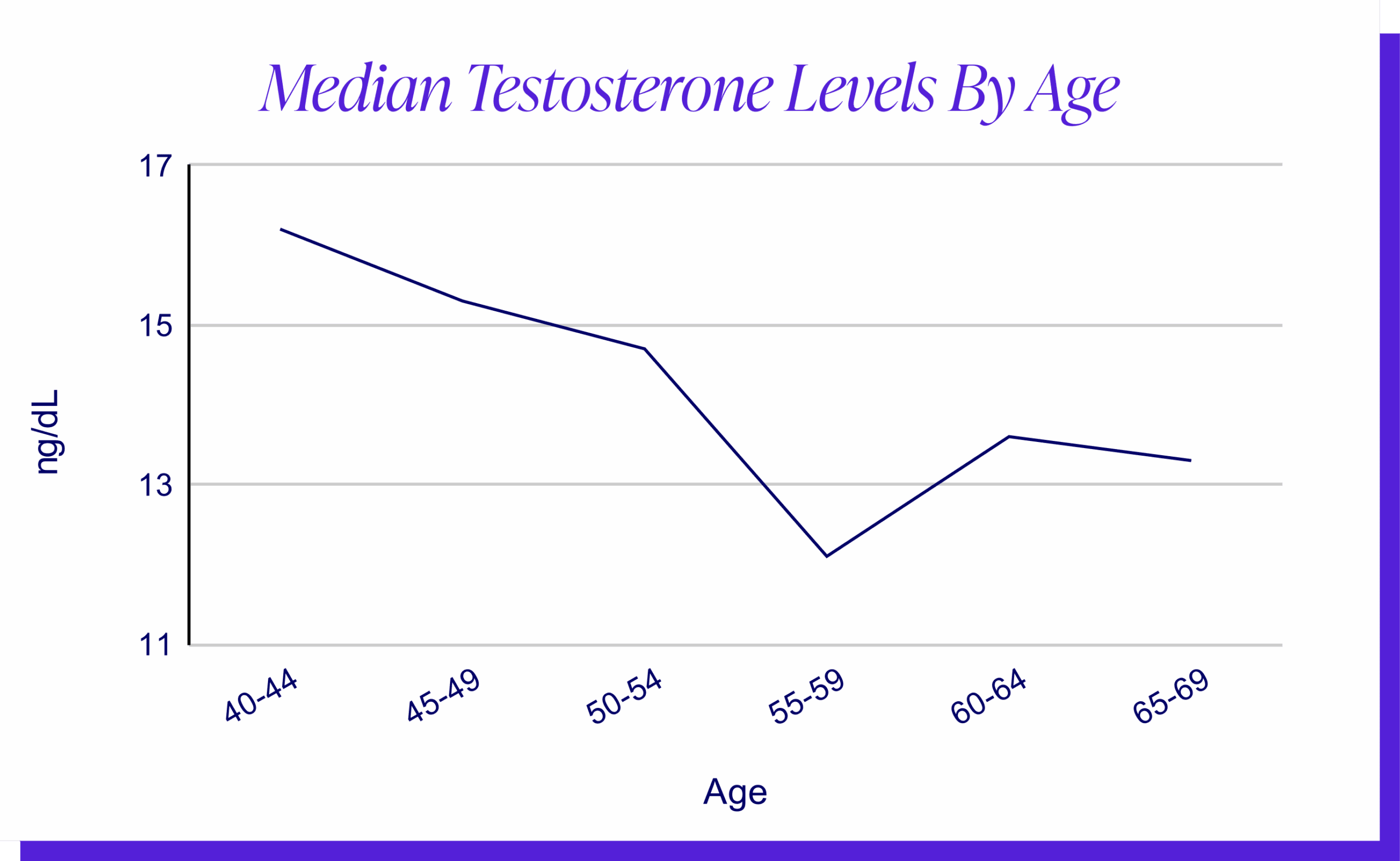
It’s important to note that testosterone declines as a result of aging, not menopause. However, its decline often coincides with perimenopause and menopause, which has created some confusion among patients and providers and has led to the misconception of testosterone therapy as a menopause wonder-drug…
What testosterone therapy can and can’t do
Testosterone for low libido
Generally supported…but with an important caveat.
Testosterone supplementation can be an effective treatment option for postmenopausal women with hypoactive sexual desire disorder/HSDD (or persistent low desire) that has not responded to traditional hormone therapy or behavioral interventions. The reason we typically want to explore these avenues before considering testosterone is that for many women, low sex drive is the result of untreated menopause symptoms like vaginal dryness or pain with sex. These symptoms are related to the loss of estrogen and progesterone, not testosterone.
It’s also worth noting that libido and sexual desire have a biopsychosocial basis, meaning we have to treat all parts of the puzzle at the same time. It’s not always related to hormones. Factors like body image issues, stress at work, and communication challenges with partners can also show up in the bedroom. It’s not always just hormones.
If, after addressing the above, disinterest in sex persists and it is bothersome, testosterone can be a good option.
Testosterone for general well-being
Not enough data to make a slam-dunk claim.
While testosterone can be a useful tool for managing low sexual desire, oftentimes when patients ask about testosterone, they’re doing so with a number of other purported “well-being” benefits in mind, many of which are being referenced widely on social media. These claims include improved cognition and mood, increased stamina, and increased bone density and muscle mass. While anecdotal reports do warrant further exploration, the current data — based on randomized clinical trials, the gold standard for establishing treatment efficacy — does not support these benefits.
A note on the limitations of women’s health research
This is often, rightly so, where frustration with the women’s health research process emerges. Patients and healthcare providers alike may find themselves feeling disempowered within a system that has historically privileged men’s health research. This is without question, and we still have a lot of catching up to do.
That said, we might take some comfort in knowing that when it comes to testosterone prescribing for women, there HAVE been good studies to support current decisions. Professor and endocrinologist Susan Davis, for instance, has dedicated her career to studying the role of sex hormones in women, and is a preeminent researcher on menopause and aging. She has led several large, international clinical trials — the very kind of research that should determine clinical practice guidelines — which have shown testosterone treatment to be effective for postmenopausal women with low libido, but not for the other benefits being promoted.
Okay, so it might not help with everything, but it can’t hurt right? That might not be the case, either…
Testosterone side effects, and why more isn’t always more
There is an increasing tendency in the menopause space to say “why not,” or “even if it doesn’t help, it can’t hurt.” This is troubling for a number of reasons, not least of which is the downplaying of risk in the name of cutting-edge clinical care. Access to limitless personal accounts and testimonials has created somewhat of a FOMO effect in menopause medicine, or fear of missing out, and we continue to see that excitement for novel therapies outpaces evidence.
In the case of testosterone therapy, what we’re talking about is not a low-risk vitamin supplement, but a medication with potential for real, often undesired side effects like:
- Acne
- Hair loss on the head
- Voice deepening
- Facial hair growth
- Enlarged clitoris
Fortunately, these effects of testosterone can be avoided with careful, low dose prescribing, but what does that look like in practice? Let’s take a look…
What responsible testosterone prescribing looks like
Off-label prescribing (yes, really)
Currently, Menopause Society guidelines include the use of testosterone therapy for the treatment of low desire in postmenopausal women, in keeping with established research. Unfortunately, there are currently no FDA-approved testosterone products for women in the United States, which is problematic for a number of reasons. (A few countries including Australia and the UK are ahead of the curve here, with formulations of testosterone for women approved and available). Sexual medicine practitioners and menopause specialists in the US who treat women through testosterone therapy will often choose to prescribe an off-label transdermal testosterone cream or gel that is applied to the skin daily. The medicine is FDA-approved for men, so it’s formulated in a way that makes it more difficult for women to use and requires mindful dosing adjustments.
Lab testing
While labs are not typically recommended for determining estrogen or progesterone dose since these hormone levels fluctuate so dramatically during perimenopause, it IS recommended that total testosterone levels are checked before treatment. Testosterone levels aren’t subject to the same dramatic ups and downs (remember…the decline is due to aging, not menopause) and bloodwork allows us to establish a clear and important picture of patients’ baseline levels. Many women have ample testosterone throughout midlife; if we add on top of that, it likely won’t actually improve sexual dysfunction — and we run the risk of those masculinizing, potentially irreversible side effects.
The bottom line
Testosterone therapy can be an effective treatment for some postmenopausal women experiencing low libido. However, widespread endorsement of testosterone for other benefits, such as improving stamina, cognition, and overall health, has muddied the waters. These claims — often presented in the name of female empowerment — are not supported by established research, and may whitewash potential side effects of testosterone, which is ultimately unfair to women. We are eager to see more research on the long-term safety of this treatment, and whether or not it may be safe and effective for premenopausal women.
At Elektra, our clinicians follow an evidence-based approach closely adhering to Menopause Society guidelines, which includes the use of testosterone therapy for the management of low desire in postmenopausal women. However, due to strict regulations and restrictions, we are currently only able to prescribe in NY. A clinical care appointment is most appropriate to determine whether testosterone would be a safe and appropriate treatment option.
READ MORE:
- Elektra Guide To Hormone Treatments in Menopause
- Elektra’s Take: Is Bioidentical Hormone Replacement Therapy (HRT) Safer for Menopausal Women?
- All About Addyi, A Non-Hormonal Treatment For Low Libido In Premenopausal and Postmenopausal Women
- Is DHEA Good For Menopause Symptoms? What to Know.
- Menopause Libido and Spontaneous vs. Responsive Desire: What’s the Connection?
- Is Vaginal Estrogen Safe? What The Science Says.