Sleep Problems
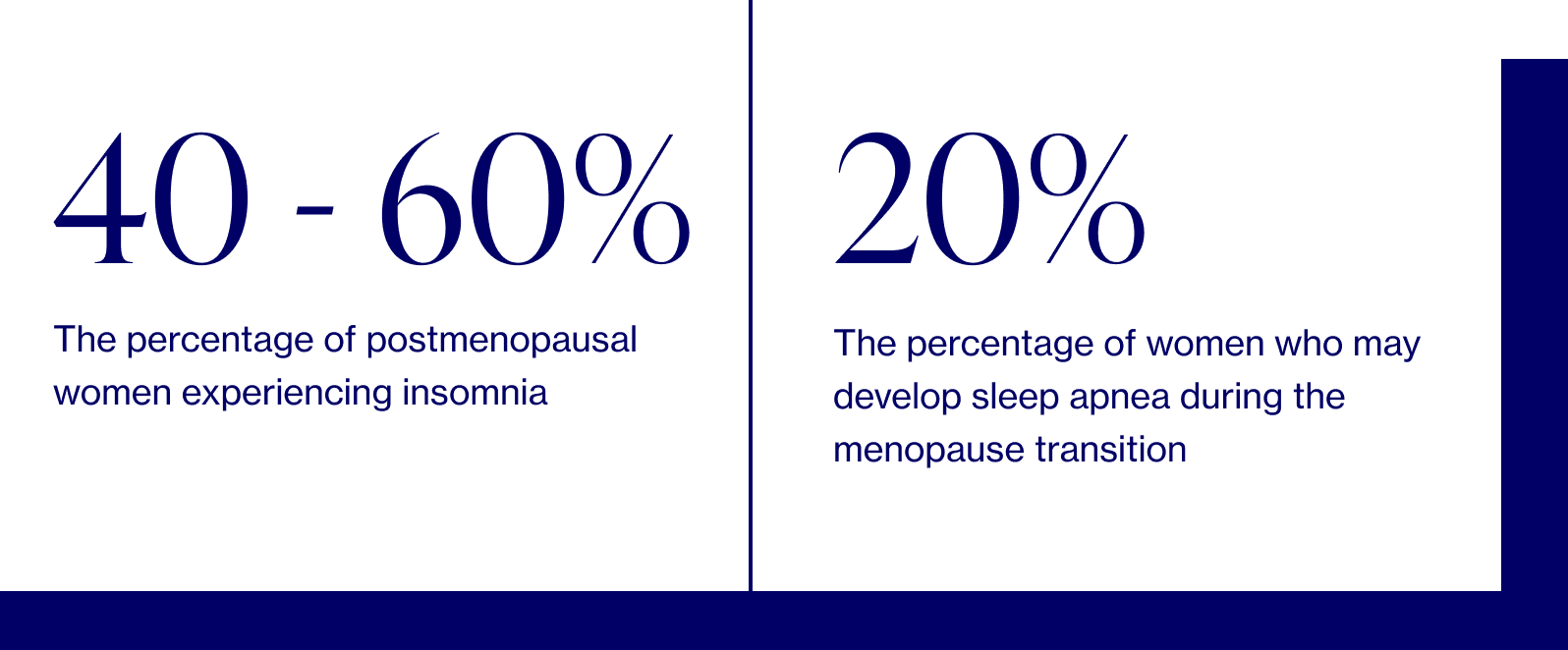
Sleep problems — i.e. difficulty falling asleep and staying asleep, waking up too early, suffering from sleep apnea (abnormal breathing, specifically extended pauses in breath) — are common perimenopausal and menopausal symptoms. Better sleep = fewer symptoms and poor sleep = worse symptoms...which, we know, totally sounds like a lose-lose situation. But it doesn’t have to be — and we’ve got the science-based tips & tricks to prove it.
The science
“Sleep problems” is an umbrella term doctors use to describe what many women experience during the menopausal transition.

Dr. Anna Barbieri, MD
Pro tip #1
Waking up in the middle of the night is as common as it is frustrating. Here’s our step-by-step approach to address middle-of-the-night scaries brought on by sleep disturbances.
1. Start with this breathing exercise.
2. If that doesn’t do the trick, try a body scan to calm you from head to toe.
3. If, after 30-45 minutes, you’re still not tired, get up and move to a chair — but keep the lights dim. Sit there quietly until you feel tired, then return to bed.
It encompasses everything from trouble falling asleep to the inability to stay asleep. Disorders such as chronic obstructive sleep apnea also qualify, which we’ll dive into in more detail below.
While hormones can play a role in sleep, not all sleep issues women experience during menopause are due to menopause-related hormones. We can’t underestimate all of the other factors that come into play: aging, stress, diet, behaviors. It’s no wonder so many women report sleep issues, even those who slept like babies for their entire adult lives.
Why does menopause affect sleep?
Hormonally speaking, there are two forces that can create the perfect storm: menopause and aging.
- Decreased melatonin: Our bodies use this natural hormone to regulate the circadian sleep-wake cycle. When levels decrease with aging, it affects the regulation of our internal clocks.
- Increased cortisol: Cortisol is a key stress hormone, and when levels increase due to aging and stress, it can prevent quality sleep.
- Decreased serotonin: When we age, the number of receptors for our “happy hormone,” our bodies use as a mood stabilizer, decreases, which may be a risk factor for anxiety and depression (both of which inhibit sleep).
- Decreased estrogen: Estrogen works behind the scenes to decrease sleep latency (aka the amount of time it takes to fall asleep) and the number of times you wake up throughout the night — in addition to increasing total sleep time. Estrogen also has a complex relationship with serotonin, so declining estrogen levels can be associated with less serotonin action. In addition, estrogen regulates our body temperatures at night. Unfortunately, as you know, estrogen levels only decrease during menopause. (*facepalm*)
- Decreased progesterone: In early perimenopause, progesterone drops even faster than estrogen does and, due to its relaxing functions, can lead to disrupted sleep, especially sleep fragmentation.Fluctuating hormone levels, in turn, cause things like hot flashes, night sweats, depression, anxiety, and stress, which also impact sleep.
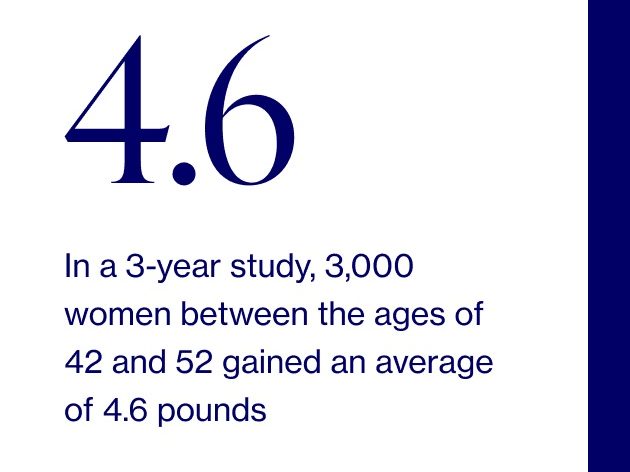
It’s a classic catch-22. You need a good night’s sleep (7-9 hours, to be exact) to feel better, but the hormonal powers that be aren’t in your favor, which makes it feel like you quite literally can’t sleep well. And when you don’t sleep well, it only exacerbates a whole slew of other menopause symptoms (low libido, weight gain, anxiety).
So if you’re thinking, this is SO unfair, we’d be right there with ya. But we’d also tell you that there are specific, totally doable ways to improve your sleep and overall quality of life that center around behavioral change and rethinking routines.
In certain cases, when you feel like you’ve tried everything under the sun and are still not getting proper sleep, your healthcare provider may step in — especially if you’re struggling with chronic obstructive sleep apnea, which is marked by abnormal breathing, specifically extended pauses in breath during sleep due to an upper airway obstruction. This is what differentiates it from the less common “central sleep apnea,” which occurs when your brain simply doesn’t send the correct signals to the muscles in charge of breathing. You may not know you have it — oftentimes, the only symptom is feeling tired even though you may be sleeping through the night. It affects postmenopausal women 2-3x more than premenopausal women due to decreases in the two primary reproductive hormones: estrogen and progesterone, and the role they play in maintaining tone in throat muscles. If you suspect that you may have sleep apnea, your doctor can screen for it and may refer you to a sleep specialist or suggest you enroll in a sleep study.
Even if you aren’t suffering from sleep apnea, it may be worth consulting your healthcare provider if you identify with one (or several) of the following:
- You experience marked daytime fatigue that interferes with work/home responsibilities.
- You worry about falling asleep while driving or doing inactive things (e.g., watching television or attending a meeting).
- You feel the need to nap most days.
What you can do
We’re all about equipping you with the know-how to understand your symptoms, and we especially emphasize the specific, tangible ways to manage them. Our goal is to empower YOU to take charge of your menopause journey, starting today.

Dr. Anna Barbieri, MD
Pro tip #2
Chronic poor sleep raises cortisol levels (a stress hormone), which causes us to wake up more often. Our favorite solution to break the cycle? Sex! Whether it’s with a partner or yourself, orgasms lower cortisol and release prolactin, which encourages relaxation and sleep.
Pro tip #3
At your wits end and ready to speak with your doctor? Keep a sleep journal for at least two weeks prior to your appointment in order to identify recurring patterns. Be sure to note your eating and drinking times, bed/wake times, as well as your general mood and state of mind.Don’t have a provider trained in menopause care? Book a visit with one of our women's health experts or email us at hello@elektrahealth.com.
A quick note about product recommendations…Elektra Health is not paid to feature any products. We just like them and think you might too, though we can’t guarantee any results.
Lifestyle
Sleep wellness is complex, with many lifestyle factors playing an important role. There isn’t a one-size-fits-all solution since it’s important to understand your unique sleep difficulties, needs, and goals. What works for you?
Nutrition & Diet
Give your diet a Mediterranean makeover
Research shows that those who adhere to a Mediterranean diet experience better quality sleep either directly (due to the diet itself) or indirectly (due to diet-related weight loss). It all comes down to the anti-inflammatory, veg-heavy, low-carb, and low-sugar properties of the Mediterranean diet. Here’s a quick primer on what is and isn’t included:
- Included: vegetables, fruits, nuts & seeds, legumes, whole grains, potatoes, herbs & spices, fish & seafood, extra virgin olive oil
- Partially included (but in moderation): poultry, eggs, dairy (cheese & yogurt)
- Rarely included: red meat
- Not included: added sugars, sugar-sweetened beverages, processed meats, refined grains, refined oils & other processed foods
Avoid large meals too close to bedtime (especially sugary, high-carb, fried, and/or spicy ones)
When consumed too close to bedtime, large meals can engage the digestive system to work on processing the meal and lead to an insulin spike that then drops (and wakes you up) about five hours later. Spicy, acidic foods can be particularly bothersome since they may trigger hot flashes or night sweats.
If you’re hungry within three hours of going to bed, reduce the quantity to a small bedtime snack. Bonus points if it has soy in it, since that has been known to minimize hot flashes and night sweats. Try a handful of nuts, dried edamame, or a glass of soy milk.
Brew a cup of chamomile tea
Chamomile is one of the oldest medicinal herbs in the world, with impressive anti-inflammatory benefits to boot. It’s rich in what’s called flavonoids, which are natural plant chemicals (aka phytonutrients) that lend fruits and veggies their vibrant hues and, according to clinical trials, induce calming effects that support sleep and help treat insomnia.
The tried-and-true … but-truly-difficult-to-do
Limit caffeine & alcohol intake too close to bedtime
Caffeine: This is nothing revolutionary — nor is it easy — but it’s worth mentioning. Caffeine is a stimulant with a half-life of 5-6 hours (or longer if you’re on certain types of medication). A “half-life” is the amount of time it takes for the quantity of caffeine in your body to be divided into two, which means after 5-6 hours, you’ll still have half the original amount of caffeine in your body. Only after 10-12 hours will it be completely eliminated.
Although people’s sensitivities to caffeine vary, it can cause difficulties in sleep onset if it’s still in your body come bedtime. As a general rule of thumb, try to avoid it after 2pm; however, if you typically go to bed on the earlier side (around 10pm), you wouldn’t want to consume caffeine after noon – 1pm(ish). And beware of hidden sources of caffeine in medications such as pain relievers, weight loss pills, diuretics, and cold medicines. There’s even small amounts of caffeine in decaf, so be sure to opt for a brand like Swiss Water, which removes 99.9% of caffeine (vs the standard 97%) in a chemical-free process.
Alcohol: When it comes to alcohol, you probably know what we’re going to say: research proves that alcohol has adverse effects on your sleep quality. Yes, a glass of wine or two can be part of a relaxing evening – and we reasonably do recommend “everything in moderation.” But if consumed too close to bedtime, even one alcoholic drink can cause fragmented sleep, delay onset of REM sleep (the dream stage), and bathroom breaks. This occurs because as alcohol is metabolized, your body experiences a rebound effect from its sedative effects during the second half of the night. This puts you into a lighter sleep stage, which means it’s easier to wake up.
If skipping alcohol entirely doesn’t feel feasible, we recommend swapping out red wine for white (red is notorious for disrupting sleep) and replacing your evening drink with a cup of herbal tea 1-2x per week to give your system a break.
Behavioral & Integrative Practices
You can eat and avoid alllllll the right foods and drinks, but without considering sleep hygiene (terrible name, we know), you’ll only get so far. By this we mean the lifestyle and behavioral practices that take place during the in-between period when you’re not sleeping. It’s a long span of time, which means a whole lot could happen that impacts your sleep. But on the flip side, there’s also a whole lot you can do about it. Below is a list of our founding MD, Dr. Anna Barbieri’s, favorite daily habits to begin incorporating. We recommend starting with one or two.
Create a wind-down routine
We have our morning routines down: it may involve exercise, coffee, breakfast, shower, or packing a lunch for the day. Whatever it is, we do it and it sets our day up for success. We need to give our wind-down the same attention and treat it the same way. Create a routine that involves practices that help you relax. Doing so will lower sympathetic activation (your body’s fight or flight system…which is not helpful for sleep!). Here’s a list of options to get started:
- A soothing bath or shower
- Cup of chamomile tea
- Stretching or restorative yoga
- Meditation, journaling, or a nightly gratitude practice
- Reading
- Brushing out your hair
- Puzzle, knitting, or some other calming activity that relaxes you
Schedule wisely
Once you build it, you need do fit your wind-down routine into your schedule. Carve out time.
Stick to a consistent bedtime
If the schedule of when we are asleep and awake varies considerably, it can throw off the physiological part of our bodies, which thrives off a 24-hour circadian rhythm. If you can, try and make this work on the weekends, too.
Keep it cool
Right around bedtime, your body temperature drops 1-2 degrees, which signals to your internal clock that it’s time to hit the hay. In doctor-speak, this is what’s called “thermoregulation.” We recommend keeping your bedroom at a cool 60 – 67°F and, if that’s not enough, trying cooling sheets made with bamboo or a cooling mattress pad or blanket for your bed.
Beware of blue light
In an ideal world, we’d all avoid screens one hour before bedtime to prevent the blue light from triggering the light receptors in our eyes which, in turn, signal the time-keeper in our brain that we’re awake. In a more realistic world, we’d try our best (but most likely end up looking at a screen on its night setting or with blue light blocking glasses).
Give sleepytime scents a whirl
Set the stage for a good night’s sleep with lavender essential oil in a pillow spray, diffuser, or drops behind the ears — and not just because it smells good. It’s scientifically proven to support relaxation, too.
Relax the mind
Wind down after a long day with meditation, breathing exercises, and sleep music/sounds — we’re big fans of Sacred Acoustics. These techniques can also help if you wake up in the middle of the night, but the key here is to practice during the day first when you’re not tossing and turning, or staring at the ceiling feeling stressed about not sleeping. This way, when you need the skill, it’ll be there.
Cognitive Behavioral Therapy (CBT) for insomnia
CBTI involves working with a sleep coach or therapist to recognize and change beliefs — including negative thoughts and worries — that impact your ability to sleep. That’s the “cognitive” part. And then there’s the “behavioral” part, which helps you develop better habits while avoiding those that inhibit quality sleep. It’s ideal for those looking to address the underlying causes of sleep struggles while working towards long-term management, and studies have proven it to be as or more effective than medication with 50 – 75% of patients attaining clinically significant sleep improvements. For information on the digital CBTI options available, refer to Sleep Foundation. You can also look into sleep coaching.
Exercise
Exercise, for the most part, is good for your sleep. In fact, studies show that people who engage in at least 30 minutes of moderate aerobic exercise may see a difference in sleep quality as soon as that very night.
However, things get a bit more complicated when you factor in type of exercise and at what time of day you engage in the activity. Here’s what you need to know.
- Avoid aerobic and/or high intensity exercise within 1-2 hours of bedtime. Instead, save those for the morning since they can delay melatonin release and negatively impact sleep. Our go-to is Fitnessblender.com.
- Engage in low intensity movement in the evening. Things like tai chi and yoga are great choices (shout-out to Melissa Wood Health!)
Supplements & Over-the-Counter Solutions
Supplements and over-the-counter solutions can be effective in supporting your sleep health…if you choose wisely. We recommend consulting with your healthcare provider first to ensure you’re using something with optimal efficacy and safety (i.e. backed by clinical research) or consulting with Elektra’s providers for medical advice.
Antihistamines
Antihistamines, such as those found in over-the-counter medications like diphenhydramine (Benadryl) or doxylamin (Unisom), commonly cause drowsiness as a side effect. While they can be taken once in a while, we do not recommend them routinely due to potential grogginess (which you don’t want extending into the next morning).
Ashwagandha
Ashwagandha is an adaptogen, which encomapsses a group of herbs that have been used in Ayurveda (traditional Indian medicine) for thousands of years. It’s derived from the roots and berries of a small evergreen shrub and helps manage levels of the key stress hormone, cortisol, which interferes with the production of melatonin.
Vitamin B6
B6, which is one of eight B vitamins, has been shown to boost serotonin levels and, as a result, help minimize hot flashes and night sweats, which themselves can lead to disrupted sleep.
Cannabidiol (CBD)
There is a growing and promising body of research specifically looking at CBD use and sleep, and there are some companies that are incorporating CBD into their sleep supplement formulations (Proper is one example, and it’s a brand with solid manufacturing practices).
It’s important to note that CBD research so far has focused on seizure disorders and anxiety. While additional benefits seem promising, we simply don’t know the specific risks and benefits, or even what is considered to be appropriate dosing. Lots of companies use it in their supplements and the amounts usually used are considered to have a low chance of side effects, but some CBD products may contain small amounts of THC (the ingredient that gives the “high”).
If you want to try CBD, doing your research is of the utmost importance.
L-theanine
Commonly found in green and black tea leaves, L-theanine is an amino acid that has been studied for its anxiety and stress-reducing properties.
Magnesium
This mineral, which is found on earth and in the human body, plays a role in over 300 biochemical reactions…sleep included. It’s found naturally in foods like leafy greens, salmon, nuts, seeds, and legumes, but many Americans don’t get enough through dietary sources.
Note: The most common side effect is upset stomach, which can be prevented by taking magnesium glycinate or magnesium L-threonate.
Melatonin
This hormone helps regulate our sleep-wake cycles, or circadian rhythms, by shortening the amount of time it takes to fall asleep, improving overall sleep duration, and increasing the time spent in REM sleep. Small amounts of melatonin are found in fruits, nuts, olive oil, and wine.
Valerian root, hops & lemon balm
Valerian root is an ancient herb whose roots have been studied for centuries to promote sleep; hops (as in beer hops) are a type of flowering plant; and lemon balm is a perennial herb from the mint family. All three have been shown in studies to aid relaxation and sleep, which is why they’re often combined in supplements and teas.
Prescription
Hormonal
Improved sleep may be both a direct and indirect benefit of hormone replacement therapy (HRT) due to its effect on estrogen and progesterone (we have receptors for both in our brain) as well as night sweats. Typically, however, HRT is not the first line of treatment for insomnia alone, and the decision along with its benefits and risks should be discussed with your doctor. If insomnia is your primary issue, we recommend behavioral, nutritional, and lifestyle solutions.
Non-Hormonal
Non-hormonal medications can be effective for acute situations of poor sleep caused by high stress or grief; however, they’re designed for occasional, one-off use only.
Keep in mind that certain medications have the potential to interact with other medications or alcohol, so it’s important to discuss with your provider and read the fine print. Also, you need to reserve at least eight hours of sleep when taking a sleep medication.
Benzodiazepines / Anxiolytics
This family of drugs is typically used for treating anxiety. Examples include alprazolam (Xanax), diazepam (Valium), and clonazepam (Klonopin), which work by enhancing the activity of GABA, a neurotransmitter that calms the activity in our brains. These medications can be habit-forming, so regular use is not recommended.
Antidepressants
Since those suffering from depression may also experience insomnia symptoms, antidepressant medications such as Trazodone may be prescribed for temporary sleep support. They work by influencing the serotonin receptors in our brain, thus reducing the time it takes to fall asleep.
Sedatives / Hypnotics
Zolpidem (Ambien) and eszopiclone (Lunesta) are two types of non-benzodiazepines that help people fall asleep faster but have little to no effect on the quality of deep sleep.
We’re always keeping an eye out on emerging research and the latest clinical studies. Subscribe to our weekly Elektra Digest for the latest, science-based info direct to your inbox. Something work well for you that’s not listed here? We want to hear it! Shoot us a note at hello@elektrahealth.com. (We’re human, promise.)
Disclaimer: This information is for general educational purposes, and should not be used as a substitute for medical advice, diagnosis, or treatment of any health condition or problem.
As with anything you put into your body, taking dietary supplements can also involve health risks. You should consult a medical professional before taking supplements and inform your doctor about any supplements, as well as any medications you already take, since there may be interactions.
References
Last reviewed 12/29/21
Lee, J., Han, Y., Cho, H. H., & Kim, M.-R. (2019). Sleep Disorders and Menopause. Journal of Menopausal Medicine, 25(2), 83.
Vahratian, A. (n.d.). Sleep Duration and Quality Among Women Aged 40–59, by Menopausal Status. Centers for Disease Control and Prevention.
Jehan, S., Jean-Louis, G., Zizi, F., Auguste, E., Pandi-Perumal, S. R., Gupta, R., Attarian, H., McFarlane, S. I., Hardeland, R., & Brzezinski, A. (2017). Sleep, Melatonin, and the Menopausal Transition: What Are the Links? Sleep Science, 10(1), 11–18.
Woods, N. F., Mitchell, E. S., & Smith-DiJulio, K. (2009). Cortisol levels during the menopausal transition and early postmenopause. Menopause, 16(4), 708–718.
Lee, J., Han, Y., Cho, H. H., & Kim, M.-R. (2019b). Sleep Disorders and Menopause. Journal of Menopausal Medicine, 25(2), 83.
How Does Menopause Affect My Sleep? (n.d.). Johns Hopkins Medicine.
Sleep Apnea - Causes & Symptoms. (2020, December 9). Sleep Foundation.
How Much Sleep Do We Really Need? (2020, December 11). Sleep Foundation.
Gunnars, K. B. (2018, July 24). Mediterranean Diet 101: A Meal Plan and Beginner’s Guide. Healthline.
Godos, J., Ferri, R., Caraci, F., Cosentino, F. I. I., Castellano, S., Galvano, F., & Grosso, G. (2019). Adherence to the Mediterranean Diet is Associated with Better Sleep Quality in Italian Adults. Nutrients, 11(5), 976.
Inflammation can lead to circadian sleep disorders. (2018, October 31). EurekAlert
Gupta. (2010). Chamomile: A herbal medicine of the past with a bright future (Review). Molecular Medicine Reports, 3(6), 895–901.
Gyllenhaal, C., Merritt, S. L., Peterson, S. D., Block, K. I., & Gochenour, T. (2000). Efficacy and safety of herbal stimulants and sedatives in sleep disorders. Sleep Medicine Reviews, 4(3), 229–251.
Alcohol and Sleep. (2020, December 11). Sleep Foundation.
Caffeine & Sleep Problems. (2020, December 8). Sleep Foundation.
Menopause & Sleep. (2020, December 10). Sleep Foundation.
What is Sleep Hygiene? (2020, December 10). Sleep Foundation.
Koulivand, P. H., Khaleghi Ghadiri, M., & Gorji, A. (2013). Lavender and the Nervous System. Evidence-Based Complementary and Alternative Medicine, 2013, 1–10.
Insomnia treatment: Cognitive behavioral therapy instead of sleeping pills. (2016, September 28). Mayo Clinic.
Exercising for Better Sleep. (n.d.). Johns Hopkins Medicine.
Van Reeth, O., Sturis, J., Byrne, M. M., Blackman, J. D., L’Hermite-Baleriaux, M., Leproult, R., Oliner, C., Refetoff, S., Turek, F. W., & Van Cauter, E. (1994). Nocturnal exercise phase delays circadian rhythms of melatonin and thyrotropin secretion in normal men. American Journal of Physiology-Endocrinology and Metabolism, 266(6), E964–E974.
SAGE Journals: Your gateway to world-class research journals. (n.d.). SAGE Journals.
Harvard Health Publishing. (2011, February). Overcoming insomnia. Harvard Health.
Hall, M. H., Kline, C. E., & Nowakowski, S. (2015). Insomnia and sleep apnea in midlife women: prevalence and consequences to health and functioning. F1000Prime Reports, 7, 7–63.
Central sleep apnea - Symptoms and causes. (2019, June 25). Mayo Clinic.
When to Call a Doctor About Sleep Disorders. (2005, April 26). WebMD.
Breus, M. J. (2018, January 11). Alcohol and Sleep: What You Need to Know. Psychology Today.
Chawla, J. (2020, April 21). Insomnia Treatment & Management: Approach Considerations, Cognitive-Behavioral Therapy, Pharmacologic Treatment of Insomnia. Medscape.
Mitchell, M. D., Gehrman, P., Perlis, M., & Umscheid, C. A. (2012). Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC Family Practice, 13(1), 1–2.