Irregular Periods
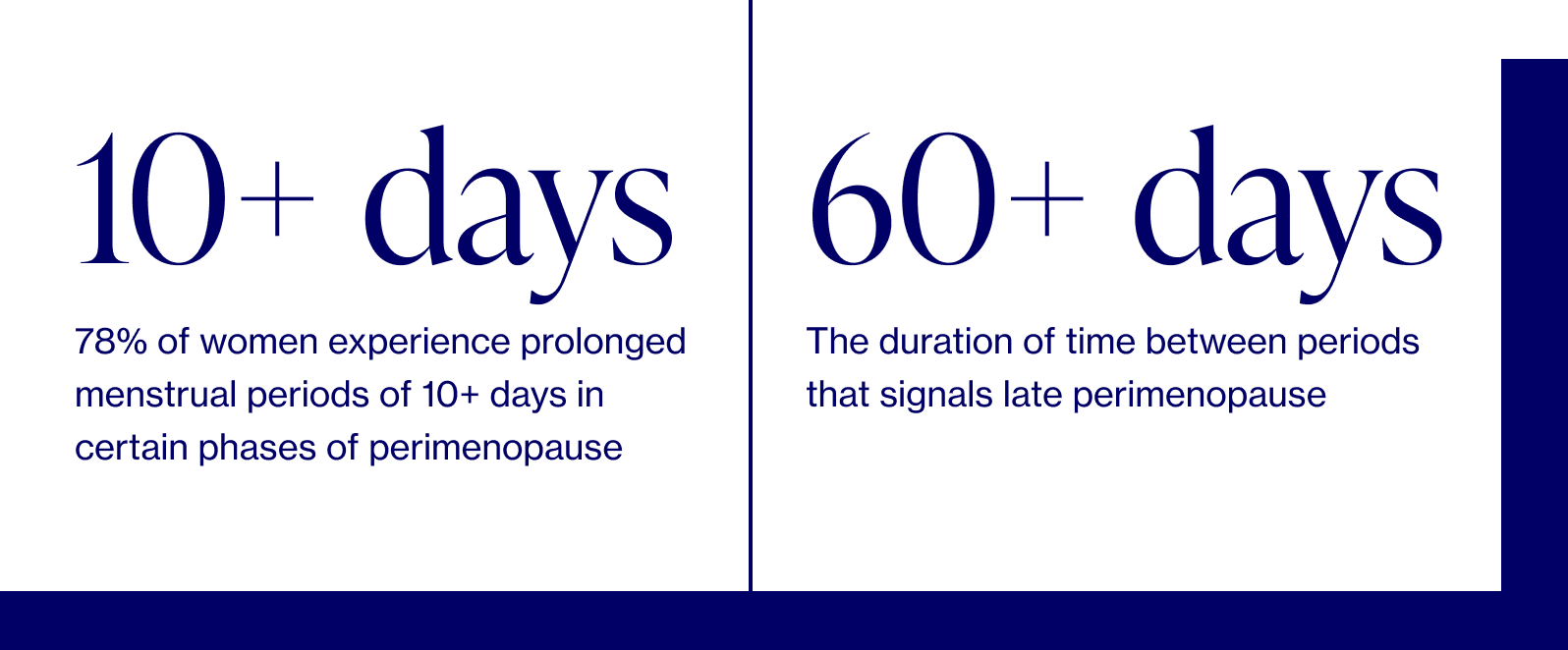
Often the first sign of perimenopause, irregular periods during this time are typically heavier and more frequent. As you progress into late perimenopause, frequency decreases before stopping altogether at menopause.
The science
Irregular bleeding is common during perimenopause. At first, cycles can be shorter by just a few days (25 vs 28 days, for example) or you may get your period every three weeks.

Dr. Anna Barbieri, MD
Pro tip #1
Before your next annual visit, track your cycle for 1-2 months to share with your doctor. Tracking specific cycle length between periods, duration of your period, and flow can help your doctor better understand where you are in the perimenopause transition, or whether there is potentially something else that should be evaulated. For example, decreased time between cycles (< 28 days) could be an early sign of perimenopause, while increased time between periods often signals late perimenopause.

Most women will experience period changes as they move into perimenopause. Changes can range from irregular cycles, abnormally heavy or prolonged bleeding (menorrhagia), and / or increasingly painful cramps (dysmenorrhea) — and yes, this can happen even if your cycle ran like clockwork before. The culprit? Hormonal changes.
How your hormones play a role
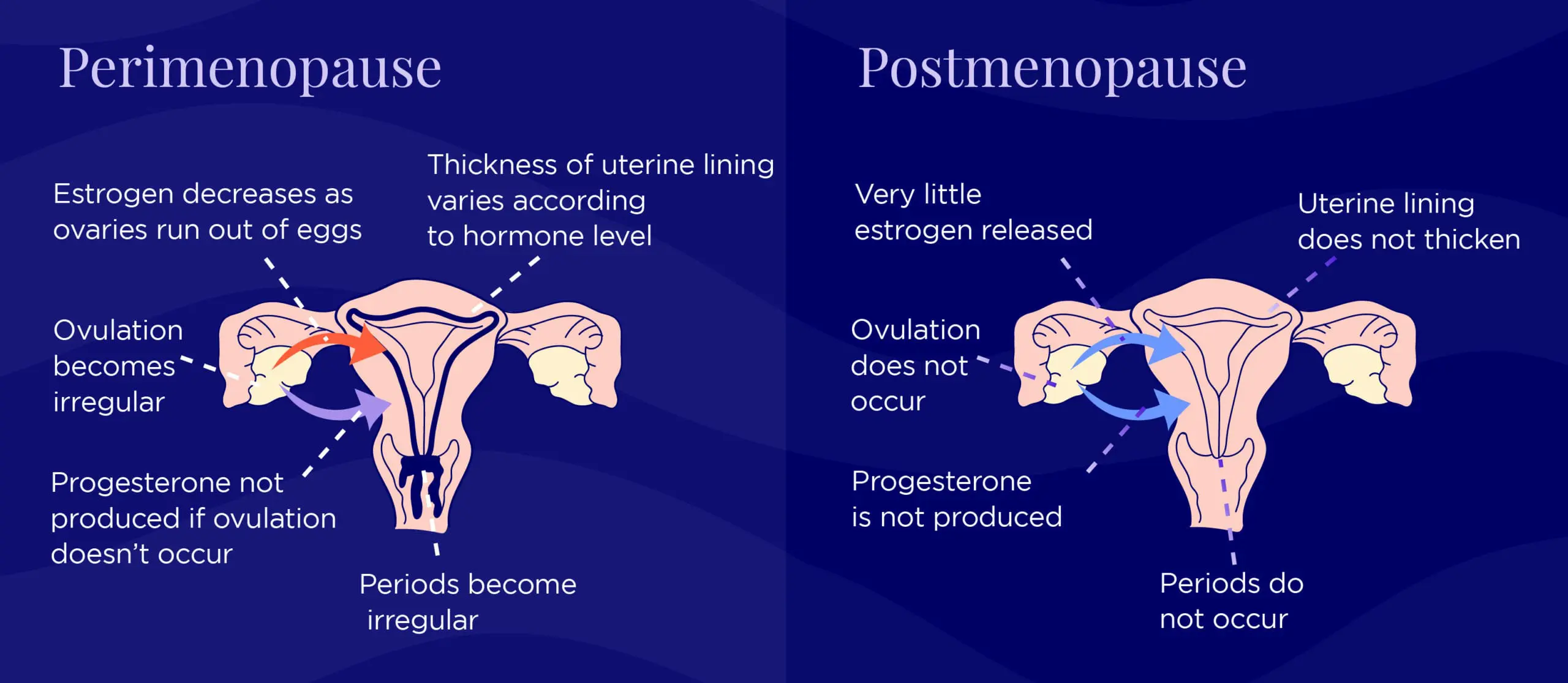
The two primary reproductive hormones for women, estrogen and progesterone, control menstruation along with a slew of other functions in our body. Among other things, estrogen causes the endometrium, or the lining of the uterus to thicken during a typical menstrual cycle. Progesterone balances estrogen by controlling the build-up of the endometrium and preparing the lining for the potential of pregnancy. When hormone levels shift and eventually decline during the menopausal transition, the result is irregular periods. Below is an example of how a woman may experience the transition, but remember: everyone is different and your experience may be different.
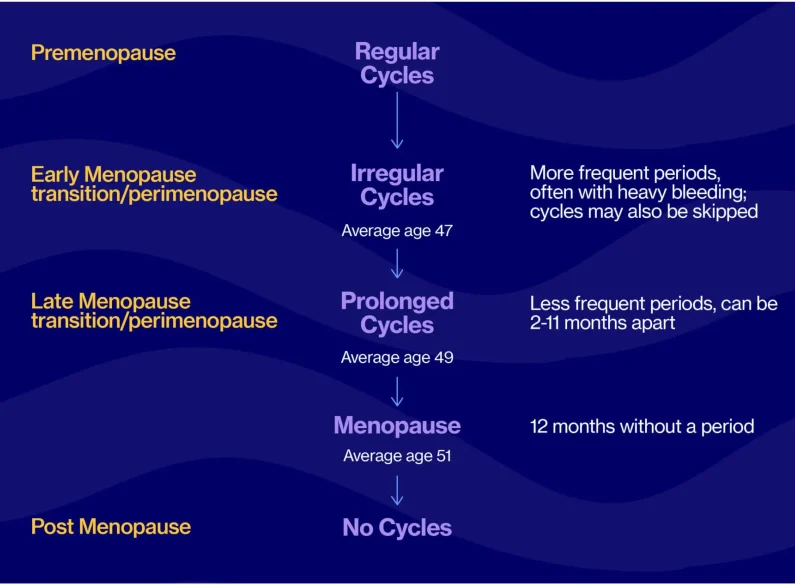
Typically, as early perimenopause shifts into late perimenopause and the last menstruation approaches, cycles become more irregular, and scarce due to declining estrogen levels, often absent ovulation, and less growth of the uterine lining. We unfortunately cannot test accurately for when that last period will come, but the average age tends to be around 51. Some women will continue to menstruate well into their 50s.
How heavy is talk-to-your-doctor heavy?
Our bodies, and our cycles, vary tremendously, but here are some benchmarks to consider, especially if this type of bleeding are new and different from your baseline:
- Soaking through 1 pad/tampon per hour for 2+ hours
- Bleeding for longer than 1 week
- Passing blood clots larger than a quarter
- Waking up at night to change a pad or tampon
Below are two other reasons you may want to seek additional medical help:
- Prolonged, heavy, or painful periods can sometimes be a result of polycystic ovarian syndrome (PCOS), polyps, fibroids, coagulation (blood clotting) problems — in which case you should definitely consult your doctor.
- Any and all vaginal bleeding post-menopause is considered abnormal and should be a sign to talk to your doctor. While the cause could very well be harmless (like dryness), it could also be a signal of a more serious medical condition, including uterine cancer. If you have postmenopausal bleeding, you need to call your doctor right away. And if you can, bring notes on the length, duration, and flow of your bleeding to that doctor’s appointment.
Oh, and one more note on irregular periods
They could very well be due to other causes outside of perimenopause and menopause, including anything that can disrupt ovulation: thyroid and prolactin abnormalities, polycystic ovary syndrome (PCOS), adrenal problems, extreme stress, illness, etc.
Periods that suddenly become irregular may require a workup to exclude causes other than perimenopause, especially for women in their early 40s. And remember, while a skipped period at 40 may mean perimenopause (or any of the culprits listed above), it can also mean pregnancy!
What you can do
We’re all about equipping you with the know-how to understand your symptoms, and we especially emphasize the specific, tangible ways to manage them. Our goal is to empower YOU to take charge of your menopause journey, starting today.

Dr. Anna Barbieri, MD
Pro tip #2
If you're having heavier bleeding, don't worry if your doctor recommends bloodwork, an ultrasound, or even a uterine biopsy. These are standard steps of a a workup for heavy bleeding and are used to identify potential other hormonal issues (like thyroid), anemia, uterine abnormalities like fibroids or polyps, and even precancerous changes in the uterine lining. Even if something is found, remember that there can be *many* solutions depending on the results.
Pro tip #3
If you’re taking NSAIDs (think Ibuprofen or Naproxen) for heavy menstrual periods and/or cramps, be sure to take them with food since an upset stomach is a potential side effect.
A quick note about product recommendations…Elektra Health is not paid to feature any products. We just like them and think you might too, though we can’t guarantee any results.
Lifestyle
Nutrition & Diet
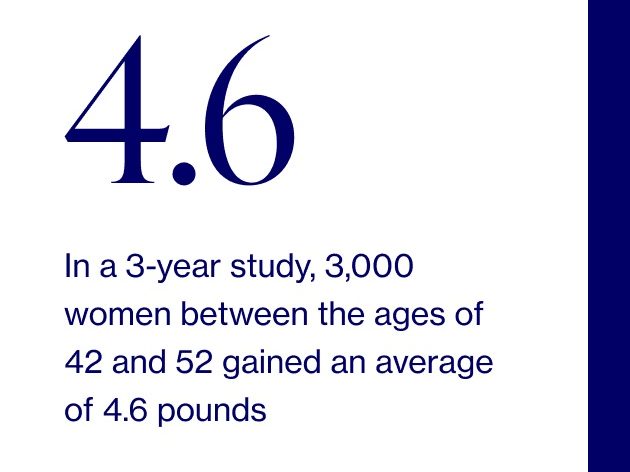
There’s unfortunately little to no research around specific foods that help with menopause-related heavy periods and irregular bleeding; however, nutrition can help if your irregular and/or abnormally heavy bleeding is due to other factors, such as obesity.
Holistic Practices
While most alternative therapies haven’t been clinically studied, the techniques below are worth trying if your heavy bleeding comes with a side of bad cramps.
- Acupuncture: When extremely thin needles are inserted through your skin at strategic points (don’t worry — it doesn’t hurt!) to reduce pain from cramping
- Acupressure: When gentle pressure is used to stimulate certain points on your body (also for cramping)
A practical tip here on absorbent period underwear. These work wonders if you’re concerned about leaking. Products such as Knix and Thinx can absorb up to 4 tampons worth of flow, but feel free to still use pads or tampons for a double layer of menstruation protection.
Supplements & Over-the-Counter Solutions
Research examining the effect of supplements on irregular and/or heavy bleeding is inconsistent and unclear at best, BUT…here comes the good news…there are two natural agents that stand out as having more evidence — although keep in mind that generally speaking, the medical approaches listed further down below are more effective than supplements.
We recommend consulting with your healthcare provider first to make sure a more effective course of action is not warranted and to ensure you’re using something with optimal efficacy and safety (i.e. backed by clinical research) or consulting with Elektra’s providers.
1. Vitex
Also known as chastetree, monk’s pepper, or Abraham’s balm, Vitex is a peppercorn-sized fruit frequently used as an herbal remedy for those experiencing frequent menstruation. By increasing progesterone, it can help with regulation of your cycles. This is an ideal supplement for early perimenopause when periods are beginning to get closer together (i.e. if you’re tracking your cycles, you’ll note the time between cycles is decreasing).
Elektra’s preferred products:
- Vitex Elixer
- Chasteberry Plus
- DIM Vitex
2. Ginger
Ginger is a flowering plant that belongs to the Zingiberaceae family and can be used fresh, dried, powdered, or in oil/juice form as an anti-inflammatory to tame heavy periods and bad cramps. (This is the same ginger we buy at the grocery store!)
Elektra’s preferred products:
- Ginger Root Drops
- Ginger Root Capsules
Keep in mind that herbal supplements have only been shown to produce effects after several weeks, so a longer commitment is required here.
A note on NSAIDs (i.e. Ibuprofen)
NSAIDs (nonsteroidal anti-inflammatory drugs) are commonly used during early-late perimenopause to regulate heavy menstrual bleeding.
Prescription
Hormonal
Research shows that hormonal treatments can help with irregular periods during perimenopause. They come in a variety of forms, with these being the two frequently prescribed options:
1. Low-dose oral contraceptives
About: Birth control pills that contain a lower dose of estrogen & progestin, which is a synthetic form of progesterone. Also a good option for women who still require contraception in perimenopause.
Phase: Early-late perimenopause
2. Sequential progesterone
About: A cyclical solution where progesterone is given in the form of progestin pills every day for a set number of days. This is repeated monthly in order to cause regular, light menstrual cycles.
Phase: Early-late perimenopause
3. Hormonal intrauterine device (IUD)
Hormonal IUDs slowly release progestin into the uterus, which thins the uterine lining, which leads to less bleeding. Some women may stop having periods altogether. IUDs can be kept in for 5+ years, and need to be inserted and removed by a provider.
Phase: Early-late perimenopause
4. Hormonal implants or injections
There are a number of available hormonal implants and injections that are available. The use of these are very personalized, and would be specific to your situation.
Phase: Early-late perimenopause
Non-Hormonal
1. Tranexamic acid
About: Also known as Lysteda, tranexamic acid affects blood clotting and can prevent heavy bleeding during menses. This shouldn’t be used by anyone who’s at higher risk of blood clotting.
Phase: Early-late perimenopause
Medical Procedures
If the above treatments are not working in your perimenopausal or menopausal journey, there are many surgical procedures available for treatment of heavy bleeding and the choice is typically individualized based on the reason for and degree of bleeding. The options range widely, from minimally invasive procedures such as uterine artery ablation, hysteroscopy, and ultrasound-guided fibroid destruction, to more more invasive treatments such as myomectomy (fibroid removal) or hysterectomy (removal of uterus).
We know surgery may sound radical, but it can be the right option in the right circumstance. We encourage you to discuss theses options and their risks and benefits fully with your doctor.
We’re always keeping an eye out on emerging research and the latest clinical studies. Subscribe to our weekly Elektra Digest for the latest, science-based info direct to your inbox.
Disclaimer: This information is for general educational purposes, and should not be used as a substitute for medical advice, diagnosis, or treatment of any health condition or problem.
As with anything you put into your body, taking dietary supplements can also involve health risks. You should consult a medical professional before taking supplements and inform your doctor about any supplements, as well as any medications you already take, since there may be interactions.
References
Last reviewed 8/27/21
Paramsothy, P., Harlow, S. D., Greendale, G. A., Gold, E. B., Crawford, S. L., Elliott, M. R., Lisabeth, L. D., & Randolph, J. F. (2014). Bleeding patterns during the menopausal transition in the multi-ethnic Study of Women’s Health Across the Nation (SWAN): a prospective cohort study. BJOG: An International Journal of Obstetrics & Gynaecology, 121(12), 1564–1573.
Perimenopause - Symptoms and causes. (2019, May 7). Mayo Clinic.
What to Expect in Perimenopause. (2019, February 1). Our Bodies Ourselves.
Bleeding after menopause: Is it normal? (2020, September 16). Mayo Clinic.
Menstrual cramps - Diagnosis and treatment - Mayo Clinic. (2020, April 8). Mayo Clinic.
Bofill Rodriguez, M., Lethaby, A., & Farquhar, C. (2019). Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database of Systematic Reviews.
Hormone Replacement Therapy for Women (HRT) | Winchester Hospital. (n.d.). Winchester Hospital.
Menorrhagia (heavy menstrual bleeding) - Symptoms and causes. (2020, July 1). Mayo Clinic.
Berger, D., Schaffner, W., Schrader, E., Meier, B., & Brattström, A. (2000). Efficacy of Vitex agnus castus L. extract Ze 440 in patients with pre-menstrual syndrome (PMS). Archives of Gynecology and Obstetrics, 264(3), 150–153.
Chen, C. X., Barrett, B., & Kwekkeboom, K. L. (2016). Efficacy of Oral Ginger (Zingiber officinale) for Dysmenorrhea: A Systematic Review and Meta-Analysis. Evidence-Based Complementary and Alternative Medicine, 2016, 1–10.
Tranexamic acid. (2019). Drugs.Com.
Cooper, K., Breeman, S., Scott, N. W., Scotland, G., Clark, J., Hawe, J., Hawthorn, R., Phillips, K., MacLennan, G., Wileman, S., McCormack, K., Hernández, R., Norrie, J., & Bhattacharya, S. (2019). Laparoscopic supracervical hysterectomy versus endometrial ablation for women with heavy menstrual bleeding (HEALTH): a parallel-group, open-label, randomised controlled trial. The Lancet, 394(10207), 1425–1436.
Bofill Rodriguez, M., Lethaby, A., & Farquhar, C. (2019b). Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database of Systematic Reviews.
Kashefi, F., Khajehei, M., Alavinia, M., Golmakani, E., & Asili, J. (2015). Effect of ginger (Zingiber officinale) on heavy menstrual bleeding: a placebo-controlled, randomized clinical trial. Phytotherapy research : PTR, 29(1), 114–119.

