Decreased Libido
Decreased libido is a common symptom of the menopause transition, and the most common women’s sexual health complaint. It's defined as a low sex drive, which manifests as little to no interest in any type of sexual activity, including self-pleasure or masturbation.


The science
Decreased libido is defined as a low desire, drive, or motivation for any type of sexual activity, as well as the lack of sexual fantasies or thoughts.

Dr. Anna Barbieri, MD
Pro tip #1
A few things to keep in mind when it comes to sexual health...sex does not require a partner and does not exclusively mean intercourse. Intimacy with yourself is *just* as important as partnered sex — and it’s healthy, too! Masturbation relieves built-up stress, helps you sleep better, boosts your mood, helps you relax, relieves cramps...we could go on and on. We’ve highlighted some of the best tools out there to help you achieve all of these benefits.

Narrowing it down to a singular cause is difficult since there can be several intersecting mental and physical factors that contribute, including:
Fluctuating hormones & physical factors:
As hormone levels shift and ultimately decline during the menopausal transition, so too can interest in sex. Interesting fact: Testosterone, the main hormone of desire, is an androgen that typically peaks in your 20s and steadily declines throughout the menopause transition, playing a major role in low libido.
Another result of hormone changes? Vaginal dryness. Because here is the thing: without sufficient estrogen and testosterone supply, vaginal tissues aren’t as moist as they once were, which leads to…you guessed it…dryness. A technical – and somewhat outdated – term for this is atrophy of vaginal tissues (a more updated and comprehensive term is “genitourinary syndrome of menopause” or, the more pronounceable acronym, GSM). Upwards of 30% of women experience it in perimenopause, and 75% postmenopause. With dryness comes painful or uncomfortable sex as well as weakened arousal and orgasm — and let’s be real: that’s not the kind of sex anyone would want to have (or should be having), which at least partly explains the low libido.
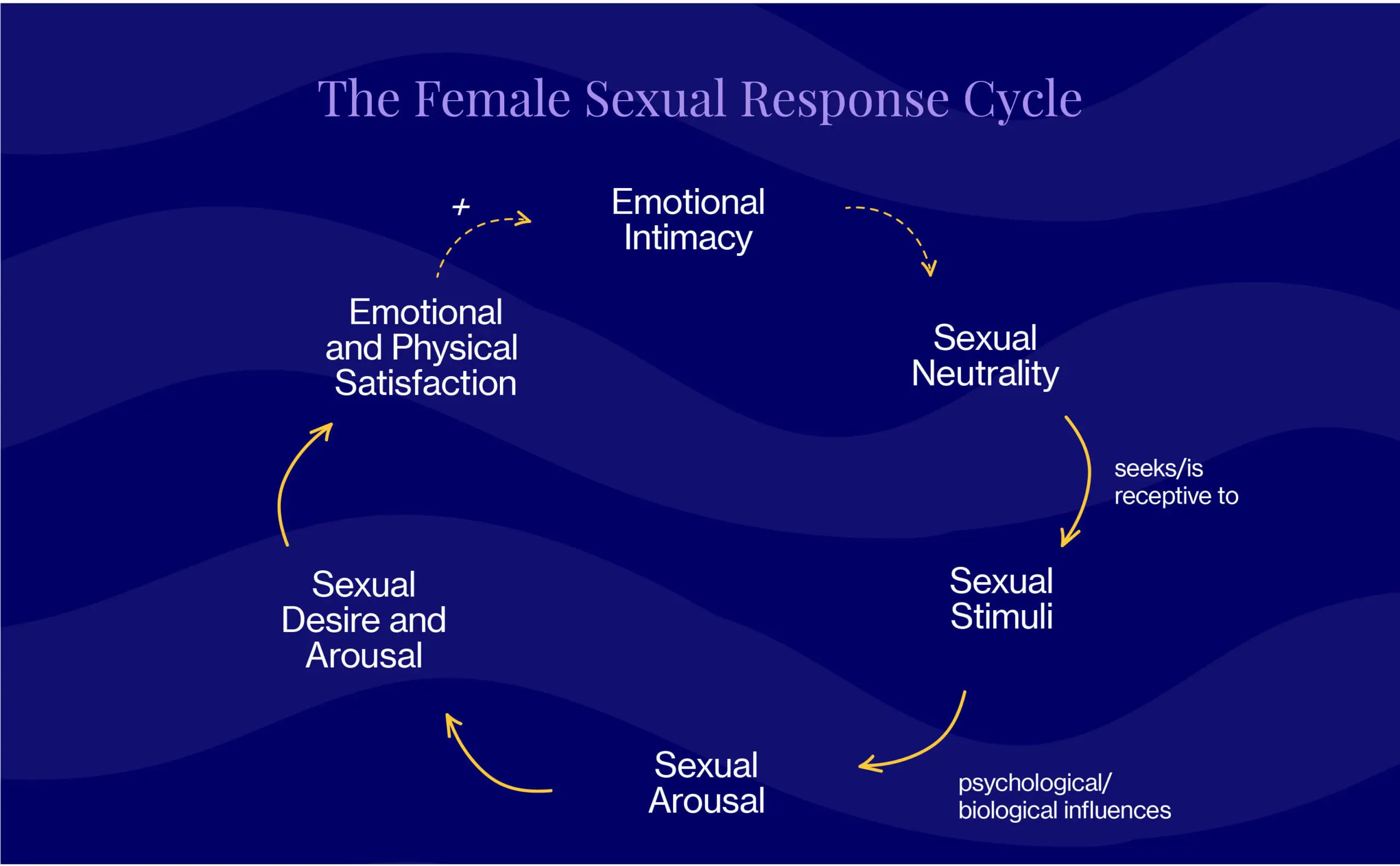
Leave it to Dr. Rosemary Basson, Director of the University of British Columbia’s Sexual Medicine Program, to prove to the world that there’s no one single reason people choose to have sex. Departing from traditional thinking, Dr. Basson created the circular, more complex model shown below, which acknowledges that a whole slew of relationship factors affect one’s willingness and ability to participate in sex. It also acknowledges that desire can be either responsive or spontaneous, and come before or after arousal. And while orgasm may contribute to satisfaction, it is not (we repeat, not) necessary for it. Oh, and you can totally enter the cycle at different points, too.
Emotional & behavioral factors:
Fatigue, stress, mood swings, relationship hurdles, and struggles with body image are things many, if not all, women experience during their lifetime. Nothing revolutionary there. But many of us don’t realize just how important of a role these emotional and behavioral factors play when it comes to intimacy, which is closeness and connectedness with a partner, either physical, emotional, or both. Intimacy is often the trigger needed for sexual desire and arousal in women.
Without emotional intimacy, the chances of sexual desire are slim. And without sexual desire, there’s no sexual activity. And repeat, and repeat.
Also worth noting is the fact that certain medications, specifically antidepressants and those used to treat heart disease and diabetes, can contribute to a decrease or loss of libido. Even some over-the-counter medications such as antihistamines (are you taking Claritin all spring?) can cause dryness and, in turn, low desire.
In some cases, low libido that persists for at least six months, negatively affects your life, and is not due to another co-existing medical/psychiatric condition or medication is diagnosed as Hypoactive Sexual Desire Disorder (HSDD). While prevalence rates vary, research suggests that HSDD affects 10% of adult females — meaning you’re 100% not alone.
Your healthcare provider may recommend FDA-approved medications, herbal supplements, and/or behavioral modifications to manage HSDD symptoms (more on that below).
What you can do
We’re all about equipping you with the know-how to understand your symptoms, and we especially emphasize the specific, tangible ways to manage them. Our goal is to empower YOU to take charge of your menopause journey, starting today.

Dr. Anna Barbieri, MD
Pro tip #2
For some, the “do it before bed” method doesn’t work, because guess what? People are usually tired then! Instead, plan sex for the morning, afternoon, or early evening when you have more time (read: longer foreplay) and more energy (read: heightened sexual desire).

Jackie Giannelli, FNP
Pro tip #3
If you have questions about sexual wellness, talk to your provider — you deserve to have your concerns heard and addressed. Unfortunately, only 40% of OBGYNS routinely ask about sexual health, so you may need to be the one to bring it up. We recommend writing down your questions in advance...and to be specific.
A quick note about product recommendations…Elektra Health is not paid to feature any products. We just like them and think you might too, though we can’t guarantee any results.
Lifestyle
Sexual desire is complex, with many lifestyle factors playing an important role (think of it less as an on-off switch, and more as a circuit board). There isn’t a one-size-fits-all solution since it’s important to understand your own body.
Take time to consider what feels good to you. What turns you on?
Below are resources our sexual medicine experts regularly recommend to revive sexual desire and improve overall wellness.
The science is clear: You can’t out-exercise a poor diet.
Apps / Websites
When it comes to erotica for libido re-stimulation, most people think visual. But audio plays an important role in desire and sexual response as well — and there’s hard science to back it up. Research shows that women are more interested than men in the broader context of the sexual narrative (compared to just the sex itself). This may be due to women’s propensity to use what’s called “mental framing” (i.e. fantasizing about different scenarios) to get turned on. Bonus points for the fact that audio is more ethical than visual, too.
- Rosy: Covers all things libido — education and erotica included
- Quinn: An audio sex platform with stories divided by theme
- Dipsea: Audio sex stories and wellness sessions with a feminist bent
Bibliotherapy
Researchers have identified a link between the act of reading erotic fiction and an increase in female sex drive for those experiencing low libido. Below are two of our top picks. Also, we really like how “bibliotherapy” rolls off the tongue!
- Best Women’s Erotica of the Year: Honest, real-life stories that span 4-8 pages and run the gamut from tame to kinky, lesbian to BDSM
- 50 Shades of Grey: This erotic book (and now, movie) series took the world by storm — seriously, 15.2 million copies sold from 2010 to 2019 made it THE best-selling book of the decade…so worth checking out (again) if you haven’t tapped into fantasy fiction lately.
Toils & oils / moisturizers
Vibrators
Vibrators work wonders when it comes to clitorial stimulation and orgasms. Some are designed for internal use, which has the added benefit of keeping the vaginal walls flexible and in shape. Here’s our take on the most popular vibrators out there — although keep in mind that which you prefer is totally personal.
The Magic Wand: Effective but large, which means it often gets in the way. That being said, it’s great for women who can’t easily orgasm but want to for solo sex.
Lush Wand: Small but mighty
Sensual Point / Jolie: Small enough to hide in hand for partnered sex
Womanizer: For those who like suction
Organic coconut oil
This natural moisturizer decreases friction via vaginal lubrication to allow for longer-lasting sex. Opt for the unrefined version, which is less processed and doesn’t undergo the same bleaching process that refined coconut oil does.
Arousal oils
Arousal oils are designed to be applied to the labia, clitoris, and inside the vagina in order to help stimulate a sexual response. Foria & Zestra are two Elektra favorites.
Communication & coaching
Communication with your partner can’t be stressed enough. Do NOT assume s/he is a mind reader. If you need help talking to your partner about sex, consider:
- Therapy with a sex counselor / therapist / health professional specializing in women’s sexual health — yes, they exist! (use ASSECT or ISSWSH to find a provider)
Supplements & Over-the-Counter Solutions
Supplements and over-the-counter solutions can be effective in supporting your sexual health…if you choose wisely. We recommend consulting with your healthcare provider first to ensure you’re using something with optimal efficacy and safety (i.e. backed by clinical research) or consulting with Elektra’s providers.
Elektra’s preferred products:
1. ArginMax
A blend of different herbs and compounds, ArginMax is thought to work by increasing blood flow and promoting muscle relaxation. Small studies have shown that Arginmax may improve sexual function in women, with improvements in sexual desire, vaginal dryness, frequency of sexual intercourse and orgasm, and clitorial stimulation.
2. Ristela by Bonafide
In three separate clinical studies, this non-hormonal formulation has been shown to enhance sexual satisfaction and increase female organsm and physical arousal in premenopausal, perimenopausal, or postmenopausal women.
3. DHEA
A double-blind study found that women who took 50 mg of this natural hormone daily reported significant increases in how often they thought about sex, how interested they were in sexual activity, and their levels of both mental and physical sexual satisfaction.
Note: If you do choose to take DHEA supplements, your hormone levels should be checked periodically by your doctor as it can affect testosterone and estrogen levels.
Prescription
Several hormonal and non-hormonal prescriptions have been proven effective in the management of low libido through the menopause transition.
Hormonal
Testosterone Replacement Therapy
Although testosterone is traditionally thought of as the “male hormone,” it plays a key role in sex drive for women. It’s not yet FDA-approved; however, but as there is substantial evidence regarding its safety and efficacy, healthcare providers are increasingly prescribing topical testosterone for postmenopausal women as an effective way to improve libido via enhanced sexual mood, nipple / clitoral sensitivity, and orgasms.
In April 2021, the International Society for the Study of Women’s Sexual Health (ISSWSH), published guidelines for the use of testosterone in postmenopausal and late perimenopausal women with hypoactive sexual desire disorder (HSDD). These guidelines give providers a clear evidence-based management strategy for when and how to use testosterone therapy.
In the world of female sexual health, these guidelines for prescribing testosterone are a big deal.
Elektra expert Jacqueline Giannelli, FNP, explains, “We are so excited to now have evidence-based and well-defined standards for prescribing testosterone for HSDD. Access to testosterone therapy for women remains an unmet need, and these guidelines are a big step in the right direction.”
Non-Hormonal
The following options have only been FDA-approved for premenopausal women; however, they can be a viable option for postmenopausal women as well.
So why don’t more women take them? GREAT question. Turns out there’s minimal, if any, awareness around these solutions (remember, only 40% of OBGYNs even ask their patients about their sex life), so it’s important to talk to your healthcare provider or Elektra for guidance first.
Addyi (Flibanserin)
This daily pill is used to treat low libido in premenopausal women. It’s shown to modestly increase sexual desire and satisfying sexual results (i.e. sexual intercourse, oral sex, masturbation, or genital stimulation by a partner), as well as reduced distress associated with a low sexual desire. Certain studies also indicate that flibanserin may aid with weight loss.
Note: Space out the consumption of alcohol with Addyi by 1-2 hours to avoid dizziness and low blood pressure.
Vyleesi (Bremelanotide)
Approved for premenopausal women with hypoactive sexual desire disorder, Vyleesi is an injected medication that has been shown to increase sexual desire and decrease distress related to low libido. Unlike daily pills, Vyleesi is only used when needed — about 45 minutes before sex.
Note: May cause nausea for some women. Women with uncontrolled high blood pressure or cardiovascular disease shouldn’t take this medication.
We’re always keeping an eye out on emerging research and the latest clinical studies. Subscribe to our weekly Elektra Digest for the latest, science-based info direct to your inbox. Something work well for you that’s not listed here? We want to hear it! Shoot us a note at [email protected]. (We’re human, promise.)
Disclaimer: This information is for general educational purposes, and should not be used as a substitute for medical advice, diagnosis, or treatment of any health condition or problem.
As with anything you put into your body, taking dietary supplements can also involve health risks. You should consult a medical professional before taking supplements and inform your doctor about any supplements, as well as any medications you already take, since there may be interactions.
References
Last reviewed 4/14/2021
Parish, S.J., Simon, J.A., Davis, S.R., et al (2021). International Society for the Study of Women's Sexual Health Clinical Practice Guideline for the Use of Systemic Testosterone for Hypoactive Sexual Desire Disorder in Women. Journal of Sexual Medicine. (Published online.)
Decreased Desire, Sexual Side Effects of Menopause | The North American Menopause Society, NAMS. (n.d.). The North American Menopause Society, NAMS.
Low sex drive in women - Symptoms and causes. (2020, March 28). Mayo Clinic.
Sexual Desire Disorder. (n.d.). Psychology Today.
Ito, T. Y., Trant, A. S., & Polan, M. L. (2001). A Double-Blind Placebo-Controlled Study of ArginMax, a Nutritional Supplement for Enhancement of Female Sexual Function. Journal of Sex & Marital Therapy, 27(5), 541–549.
Bonafide. (n.d.). Ristela Information for Healthcare Providers.
Genazzani, A. R., Stomati, M., Valentino, V., Pluchino, N., Potì, E., Casarosa, E., Merlini, S., Giannini, A., & Luisi, M. (2011). Effect of 1-year, low-dose DHEA therapy on climacteric symptoms and female sexuality. Climacteric, 14(6), 661–668.
Davis, S. R., Baber, R., Panay, N., Bitzer, J., Perez, S. C., Islam, R. M., Kaunitz, A. M., Kingsberg, S. A., Lambrinoudaki, I., Liu, J., Parish, S. J., Pinkerton, J. A., Rymer, J., Simon, J. A., Vignozzi, L., & Wierman, M. E. (2019). Global Consensus Position Statement on the Use of Testosterone Therapy for Women. The Journal of Clinical Endocrinology & Metabolism, 104(10), 4660–4666.
Ayres, B. (2020, January 8). Testosterone Replacement Therapy for Women. BodyLogicMD.
Kornstein, S. G., Simon, J. A., Apfel, S. C., Yuan, J., Barbour, K. A., & Kissling, R. (2017). Effect of Flibanserin Treatment on Body Weight in Premenopausal and Postmenopausal Women with Hypoactive Sexual Desire Disorder: A Post Hoc Analysis. Journal of Women’s Health, 26(11), 1161–1168.
Sexual Health & Relationships. (n.d.). ACOG.
Female sexual dysfunction - Symptoms and causes. (2018, September 6). Mayo Clinic.
Female Sexual Interest/Arousal Disorders. (n.d.). The Sexual Psychology Laboratory | The University Of Texas At Austin.
Basson, R. (2002). Rethinking low sexual desire in women. BJOG: An International Journal of Obstetrics and Gynaecology, 109(4), 357–363.
Vaginal Dryness - an overview | ScienceDirect Topics. (n.d.). ScienceDirect.
Hypoactive Sexual Desire Disorder. (2020, June 26). American Sexual Health Association.
Masturbation Effects on Your Health: Side Effects and Benefits. (n.d.). Healthline.
What we don’t talk about when we don’t talk about sex. (2012, March 22). ScienceDaily.
Rupp, H. A., & Wallen, K. (2007). Sex Differences in Response to Visual Sexual Stimuli: A Review. Archives of Sexual Behavior, 37(2), 206–218.
Herbenick, D., Fu, T.-C. J., Arter, J., Sanders, S. A., & Dodge, B. (2017). Women’s Experiences With Genital Touching, Sexual Pleasure, and Orgasm: Results From a U.S. Probability Sample of Women Ages 18 to 94. Journal of Sex & Marital Therapy, 44(2), 201–212.
Fifty Shades of Grey Was the Best-Selling Book of the Decade in the U.S. (2019, December 18). The NPD Group.
Palaniappan, M., Mintz, L., & Heatherly, R. (2016). Bibliotherapy interventions for female low sexual desire: erotic fiction versus self-help. Sexual and Relationship Therapy, 1–15.
Will DHEA Improve Your Well Being and Sexuality? (2018, May 22). Verywell Health.