Perimenopause 101:
What You Need to Know
Learn the symptoms and causes of perimenopause, how it fits into the overall menopause journey, and what solutions (lifestyle & medical) there are to manage it.
The science
You’ve likely heard the term menopause before...but what about perimenopause?

Dr. Anna Barbieri, MD
Pro tip #1
For many, PMS kicks it up a notch during perimenopause, which often means exacerbated emotional symptoms, mood swings, and irritability. This is where mind/body practices like meditation can be helpful. Supplements can help, too, such as Seronal for emotional symptoms, and PMS Support for physical.
Pro tip #2
It’s natural to wonder when the menopause transition might happen. Until tests can provide more accurate and reliable answers, we recommend asking mom/aunts/sisters/[insert close female relative here] since timing of the menopausal transition is often genetic. We know this may not be an option for everyone — if that’s you, don’t sweat it. That’s what Elektra’s experts are here for!
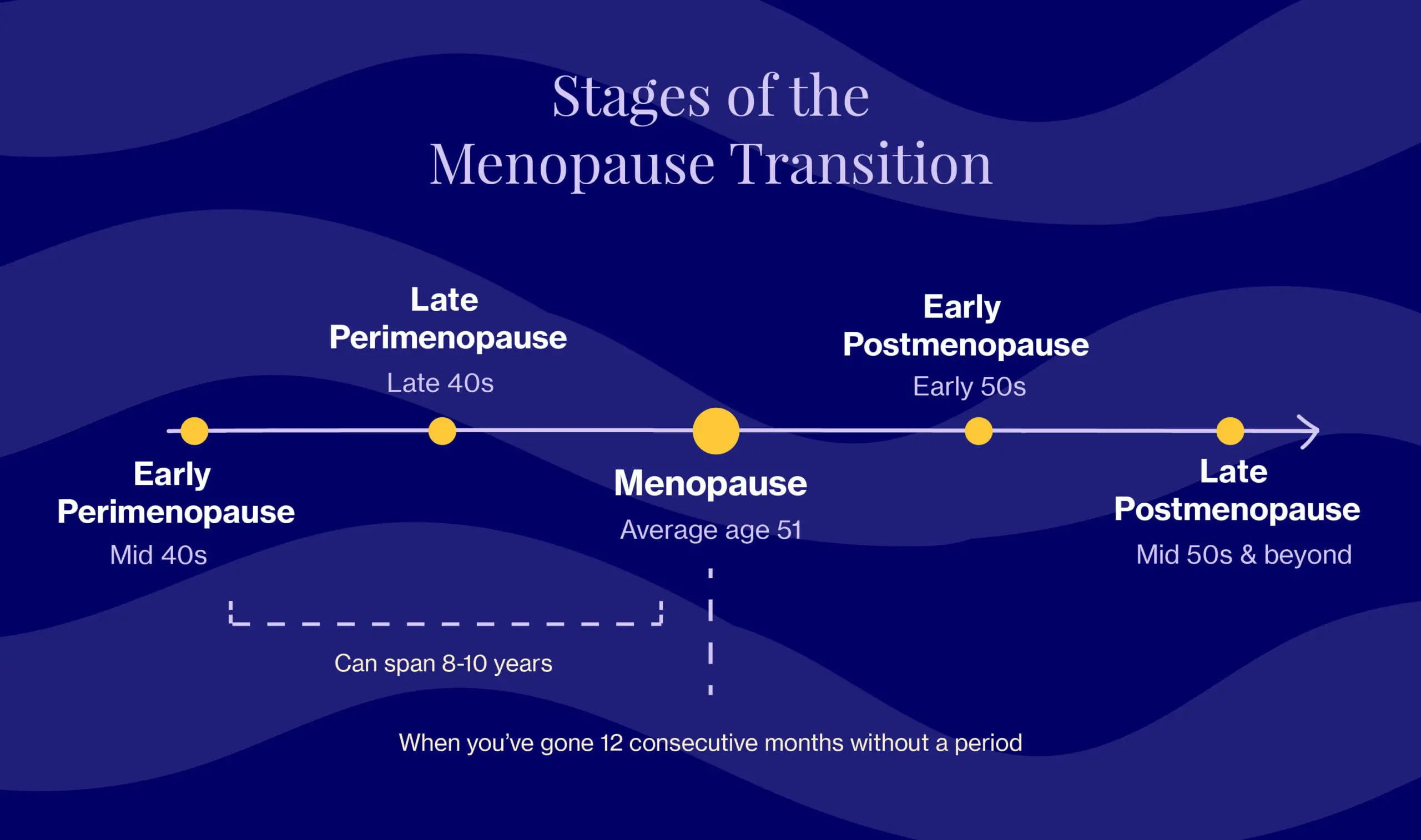
Most of us — even if we’re supported and informed — are thrown off when we hear this less-well-known word, which literally means “around menopause.” It’s used to describe the transition period between the onset of your first symptoms and the onset of menopause, which is technically marked by 12 consecutive months without a period (you can read more about that here). A doctor would say that you’re “in perimenopause” when cycles are irregular (i.e. varying by 7 days from your baseline, for example, a cycle of 33 days followed by a 26-day one) or when we skip cycles altogether.
If you’re thinking to yourself… WHAT?!…you’re not alone. Now’s as good a time as any to familiarize yourself with the start of this journey and begin building healthy habits for the years to come.
Knowing what’s happening in your body and why it’s happening is so powerful. When armed with this information, we can be proactive and preventive — and if we need support or help, we know where to go.
Never underestimate the advantage of preparation when navigating the menopause transition.
When, how & why
Perimenopause can be wildly unpredictable. Periods change dramatically, becoming heavier and more frequent, or they can go in the other direction. It’s generally a confusing time that catches a lot of us by surprise (so no, it’s not just you).
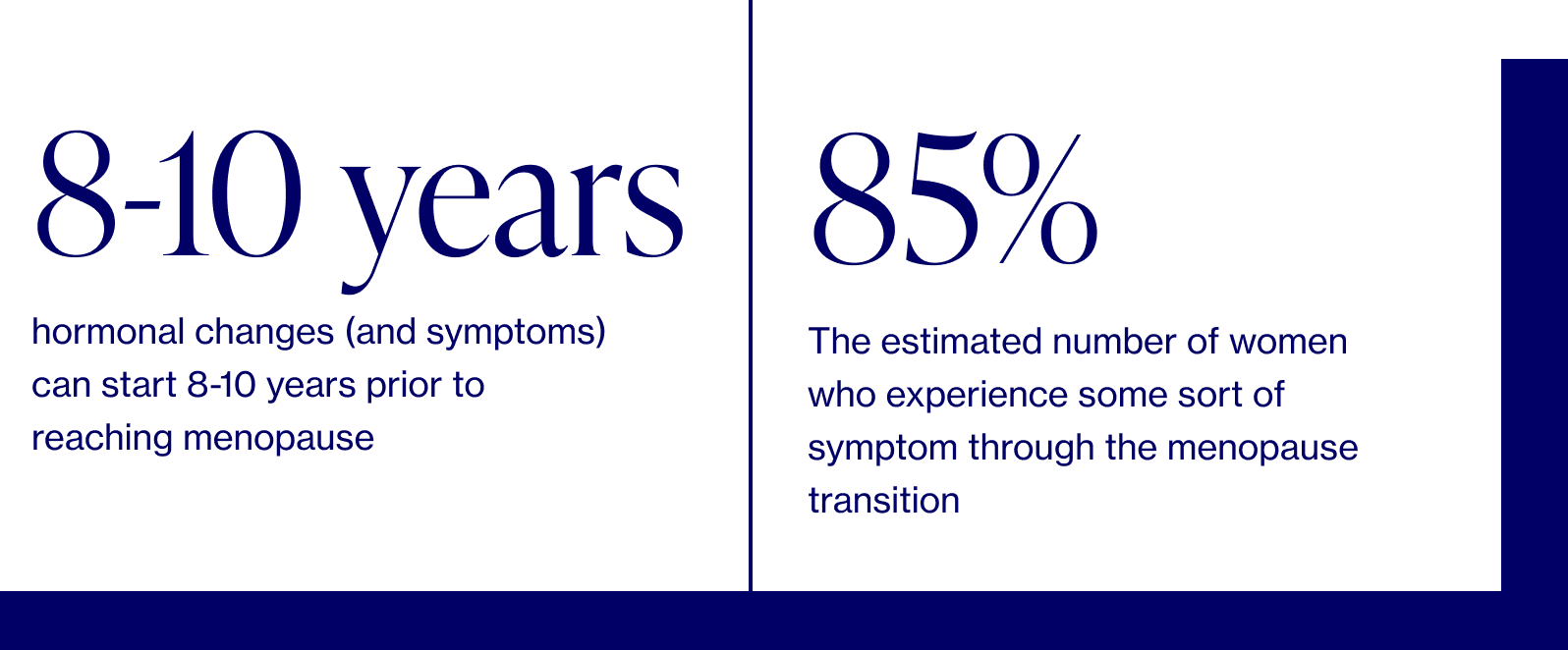
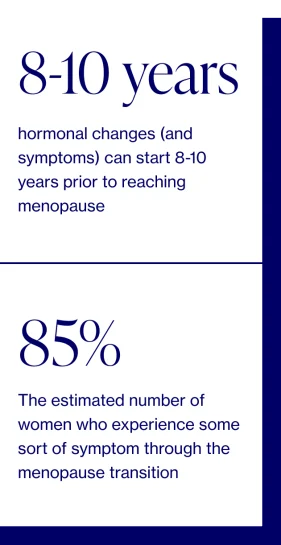
The transition in its entirety takes 8-10 years to move through, and while most of us will start in our mid-40s, some may begin years earlier. Perimenopause is often broken down into two general phases: early perimenopause (when periods can still be regular, which causes some confusion) and late perimenopause (marked by skipped and/or irregular periods — more aligned with what people typically think of when they hear perimenopause or menopause).
The takeaway? There’s no such thing as a one-size-fits-all experience. Hormonal changes, and the way symptoms show up, are anything BUT linear.
Like timing, perimenopause symptoms can vary, and each woman’s experience will be unique. We do know, however, that there may be certain racial and ethnic differences. One study in particular showed that African American women experience the worst vasomotor symptoms (hormone-related temperature dysfunction, e.g., hot flashes and night sweats), while Asian women reported the most mild.
Perimenopause symptoms: what to expect
It’s common to mistake the telltale signs of perimenopause — think hot flashes, night sweats, and mood swings — for those of menopause. But here’s a surprising fact: for many, these symptoms actually start to subside once we reach menopause, which means the worst may very well by over by this point (*cue the sigh of relief*).
Below are common symptoms that signal the beginning of perimenopause, all of which can be traced back to changing hormone levels. But remember, not everyone will experience these symptoms. Our goal here is to empower you with knowledge to manage the symptoms IF (key word) you do indeed experience them.
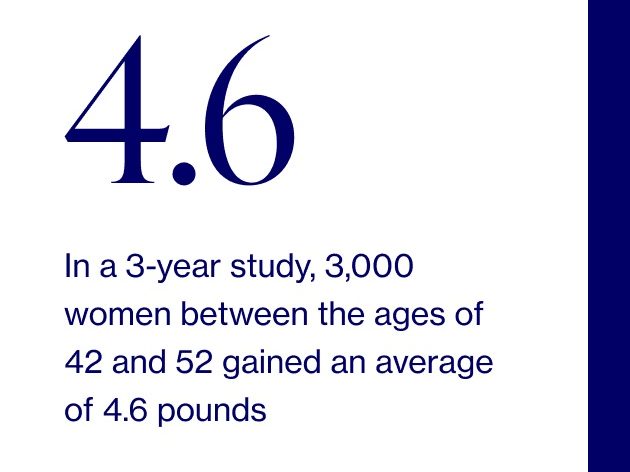
- Weight gain
- Worsening PMS with both emotional & physical changes (e.g., breast tenderness and heightened anxiety)
- Irregular periods, which is an umbrella term that can encompass short or skipped menstrual cycles and heavy bleeding (often one of the earliest symptoms)
Throughout the remainder of your journey, you may notice a number of the following perimenopausal symptoms (but not always, and not all at once): hot flashes and night sweats, irregular periods, difficulty sleeping, emotional changes (e.g., irritability, mood swings, and mild depression, especially before your period), difficulty with concentration and short-term memory, aka "brain fog," vaginal dryness and/or discomfort during sex, and dry skin.
It sounds like a lot, we know, but we’ve broken down everything you need to know about every symptom — big and small — to empower you with science-based know-how and actionable solutions.
FAQ about perimenopause symptoms
Are the symptoms constant for the entire duration of menopause?!
It depends. Some symptoms come and go and others are more constant. What you can expect, however, is for symptoms to peak about 1-2 years prior to the onset of menopause due to an accelerated drop in estrogen levels.
How long will these symptoms last?
Typically five years — but remember, the perimenopausal experience isn’t one-size-fits-all for every woman again. Some may only experience a change in their period when nearing menopause, while others will experience it for upwards of 10 years.
Are these symptoms *always* due to perimenopause?
Not always, no. There are several common conditions, including thyroid abnormalities and even medication side effects that can cause similar symptoms, so be sure you are properly evaluated by your healthcare provider.
Is there a test for perimenopause?
Yes and no…it’s complicated. Doctors may order tests to check your hormone levels and thyroid function, but it’s imperfect at best since hormones fluctuate all. the. time. during perimenopause.
The low-down on hormones during perimenopause…what’s really happening?
Okay, so here’s what we know so far: hormonal fluctuations are to blame for the symptoms listed above. Great, but that doesn’t really help us. What does is diving into the science behind the symptoms which, in turn, helps us better cope with them. So stick with us…we’re breaking it all down below.
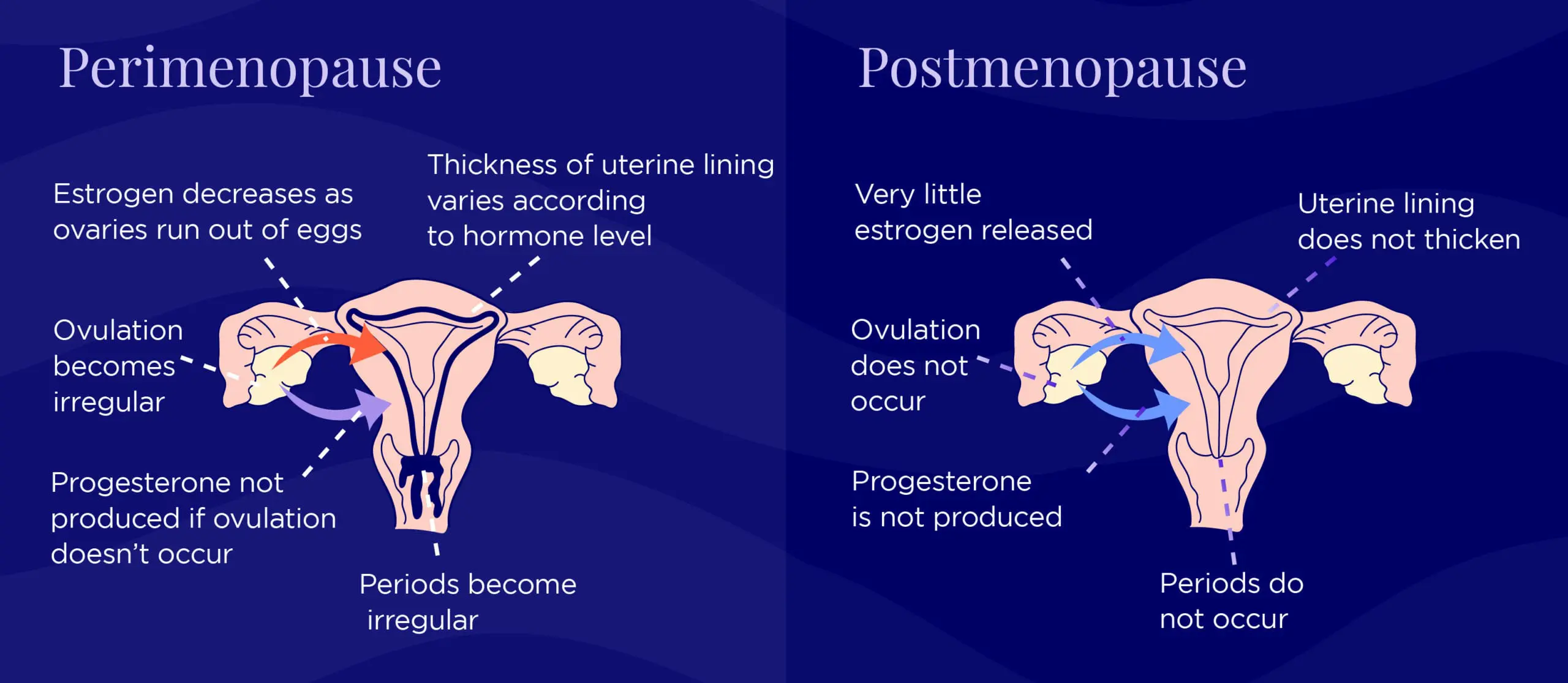
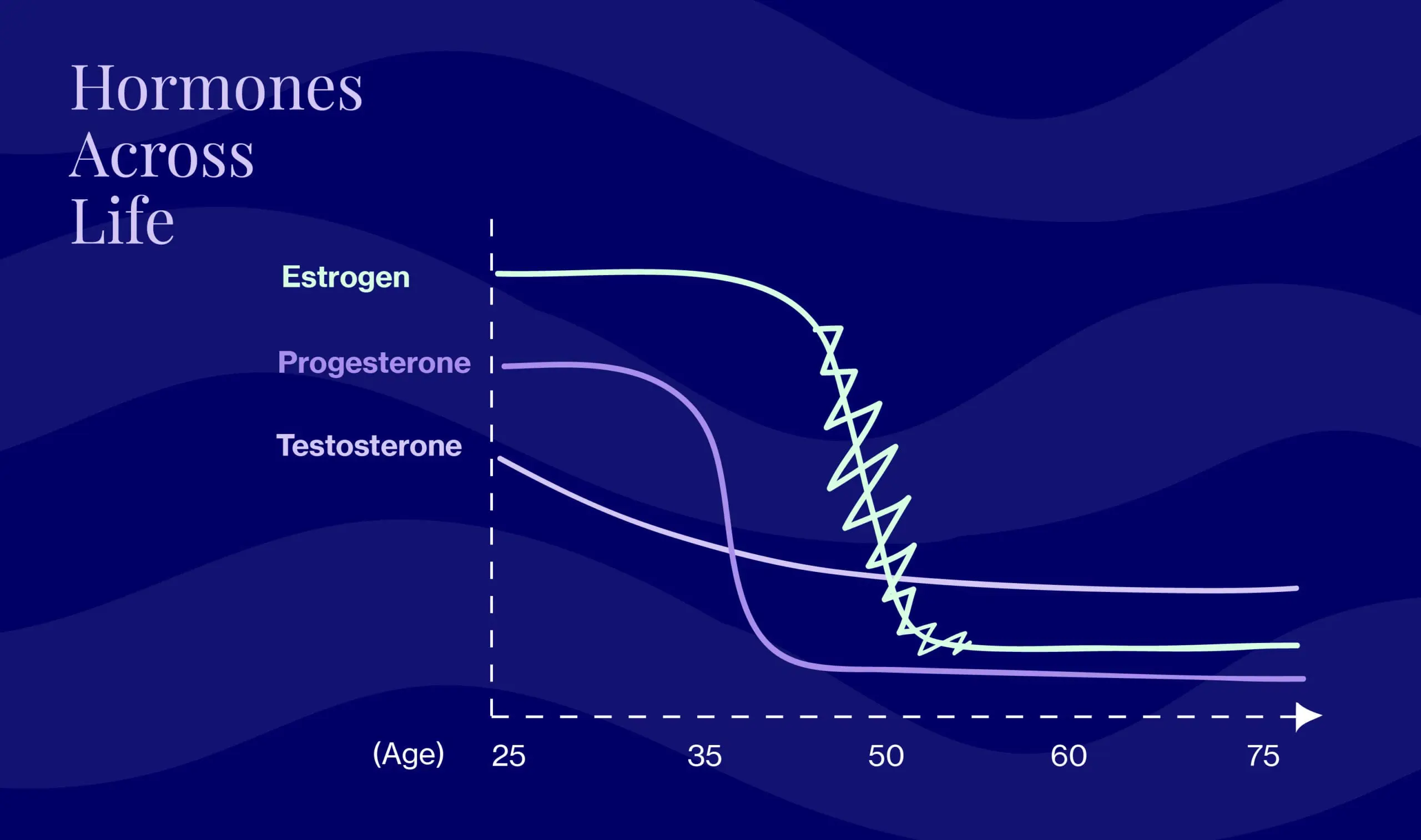
In our 20s and 30s (i.e. during premenopausal cycles), hormones enjoy a predictable ebb and flow. And in postmenopause, it’s low but steady. But the in-between perimenopausal period is marked by one long hormonal fluctuation, with levels of the two key female hormones (estrogen and progesterone) varying quite a bit. Progesterone starts to decline first, followed by estrogen, which fluctuates quite a bit as it does so. Testosterone is involved here as well, and slowly declines. So picture a rollercoaster – those are your hormones! And the rest of you is along for the ride. But those aren’t the only hormones that play a role.
Pre-menopause, FSH (follicle-stimulating hormone) and LH (luteinizing hormone) work together to produce a period. FSH causes eggs to mature in the ovaries, then LH triggers the egg’s release. During perimenopause, FSH levels fluctuate significantly, which means things get out of whack.
Wondering what hormones you should keep an eye on and/or test to determine (around) when you’ll hit menopause?
Estrogen: Menopause occurs when ovaries don’t produce enough estrogen for ovulation (which means no periods).
FSH: Although FSH was once considered the “test” for menopause, it’s not the most useful in perimenopause. Levels vary far too much to rely on it as a predictor of the last period.
AMH: Now, doctors look to AMH (the anti-mullerian hormone) to gauge the level of remaining egg cells — aka “ovarian reserve,” in doctor speak. AMH decreases with age until it becomes essentially undetectable around menopause. There are currently AMH tests in development, which could be used to assess whether a woman’s last period will occur in the next 18 months or so (via a blood test). Even though it’s possible to do an AMH test now, we don’t know that it can accurately ballpark your menopause “ETA”. So for the time being, AMH testing is not a typical part of the menopausal hormonal assessment.
What you can do
Perimenopause treatments

Dr. Anna Barbieri, MD
Pro tip #3
Head’s up that you can still get pregnant if you’re perimenopausal, so using birth control is important if that’s something you’re hoping to avoid. You’ve got options, including condoms, IUDs, and birth control pills (bonus points for the pill — it has the added benefit of evening out hormone fluctuations. One thing to keep in mind, though, is that it can be hard to gauge when menopause is coming if you’re on the pill.).
Common perimenopause medications and treatments include temporary low-dose birth control (oral contraceptives) and other hormone therapies. That said, many doctors will suggest lifestyle changes before or in addition to medication. In fact, studies have shown that women with healthy lifestyles experience fewer perimenopause symptoms and are better able to cope with those they do — but it’s still good to know that treatments are available. As with all medications, healthcare providers should factor in risks, benefits, individualized needs, and health history when planning treatment.
At Elektra, we pride ourselves on our holistic approach.
Combining traditional and integrative medicine, we take into account your physical and emotional health needs as well as goals and preferences in order to manage perimenopause (and beyond) while optimizing for long-term health and wellness.
Lifestyle changes for perimenopause
We’re all familiar with the tried-and-true healthy lifestyle recommendations — eating plenty of veggies and sticking to whole foods, getting sufficient sleep, limiting alcohol, avoiding tobacco, reducing stress, exercising regularly (both aerobic and weight-bearing). Those 100% still apply here. While striving to live, eat, and exercise healthier, we’d also remind you to be kind to yourself! Emily Dickinson said it best…”One step at a time is all it takes to get you there.” A little cheesy, but true.
We recommend building a “menopause support team.”
Start by reviewing the list of symptoms, recording your experience with each on a scale of 1-10 (least disruptive to most disruptive), and prioritizing which to tackle first. Bring this list to your next doctor’s appointment and discuss with your doctor (if you don’t feel like your doctor is listening to you, then find a new doctor!). Having a doctor on your team who knows menopause is important. Elektra is ready to help and you can email [email protected] for help finding a local option.
In addition to your medical team, you need your personal cheerleaders.
We encourage you to reach out to your confidants for support. Whether you just need someone to talk to or are looking for more concrete help (i.e. someone who’s at the ready if, say, sudden hot flashes make you want to stick your head in the freezer), start the conversation: I’m experiencing some symptoms, I think it’s perimenopause, and I need some support to get through this. We know there is still stigma and misunderstanding around the topic of menopause (hence Elektra Health!), but you owe it to yourself to not to experience this alone. And if one of your confidants is a woman in her mid-late 40s, she will likely have many of the same questions as you!
At any given moment, 50 million or more women in the U.S. are experiencing menopause, and a whopping 16% never discuss it with anyone at all. That needs to change!
Where to start
Take stock of your lifestyle. How much do you exercise? How do you manage stress? Do you sleep well at night? How’s your general eating habits? These 4 factors can play a HUGE role in how you feel as you move through the menopause transition, and it’s never too late or too early to start making changes. Here are Elektra’s founding physician, Dr. Anna Barbieri, MD’s top recommendations:
Diet
- Limit, as much as you can, processed foods and added sugars (and processed = anything that comes from a package, made with white flour, or added sugar)
- Diversify your diet with a wide range of whole foods, especially veggies and healthy fats (e.g., olive oil, avocados, nuts like almonds & walnuts, and fatty fish)
- Increase intake of organic whole soy products and flaxseed, both of which boast mild estrogenic effects
Exercise
- Add on strength training to maintain your lean muscle mass
- Never underestimate the power of a power walk – it’s a great, low-impact exercise that can get you outside and help manage stress
- Move as much as you can, as often as you can, throughout the day
Sleep & Stress
- Aim for at least 7 hours of sleep per night.
- Make sleep a priority because it plays such an important role in overall health. If it’s an issue for you, don’t just learn to live with. .
- Meditate, get outside, knit, go for a jog, read…do whatever you need to do to manage stress on a daily basis, even if it’s just for a few minutes.
All of these are important, but if this all seems overwhelming and you need to choose an area to focus first, go with diet. Building healthy eating habits now will help you through menopause and well beyond.
“There isn’t one perfect diet for everyone,” explains Dr. Barbieri. “But the common themes are plant-heavy and whole food, with low refined carbohydrates and sugar. At the end of the day, it’s about balance — the ability to maintain a healthy, sustainable change over a long time is more important than eating perfectly for just a couple of days.”
"I love seeing the tremendously beneficial effect a dietary change can have while being aware that we do not cross over into obsession and rigid patterns" -Dr. Barbieri
Along with lifestyle changes to help manage menopause symptoms, there are integrative options like supplements, prescription medications, and more. As you go through Elektra’s guides to the different symptoms, you’ll find concrete information and recommendations you can use to take charge of your hormonal health and live your best life
For too long, too many of us have entered perimenopause without the tools and resources we need to thrive, which means this 8-10 year journey is experienced in a way that’s deeply isolating, lonely, and scary.
Arming ourselves with knowledge can make all the difference - not just for perimenopause, but menopause, too.
This way, we can understand what the heck is actually happening with our hormones and just how differently perimenopause may look and feel for different women. And when we do that, we eliminate the fear of the unknown and walk away empowered to tackle perimenopause with the same badass strength and perseverance that we’ve used to overcome everything that’s come our way beforehand.
Ready? We are, too.
Disclaimer: This information is for general educational purposes, and should not be used as a substitute for medical advice, diagnosis, or treatment of any health condition or problem.
As with anything you put into your body, taking dietary supplements can also involve health risks. You should consult a medical professional before taking supplements and inform your doctor about any supplements, as well as any medications you already take, since there may be interactions.

