Menopause 101: What You Need To Know
Learn the symptoms and causes of menopause, how it fits into the overall menopause journey, and what solutions (lifestyle & medical) there are to manage it.


The science
For a good portion of our life, menopause is one of those “out of sight, out of mind”-type things..

Dr. Anna Barbieri, MD
Pro tip #1
We’re big fans of flexing the self-love muscle. Next time you look in the mirror, tell yourself that you love yourself. However silly it may sound at first, trust that the way you speak to yourself impacts your perception of self, especially as your hormones impact your relationship with your body. The more you do it, the easier it’ll get, just like any habit.
Of course we all know it’ll happen eventually, but it just seems SO far off…until it isn’t. Out of nowhere, it sneaks up on us and then — surprise! — our bodies are changing and our hormone levels are out of control.
Sound familiar? Trust us, you’re not alone — but you are in the right place. Below, we’re breaking down what you need to know about what to expect and how to manage symptoms in order to live well through all of the stages of menopause and beyond.

When, how & why
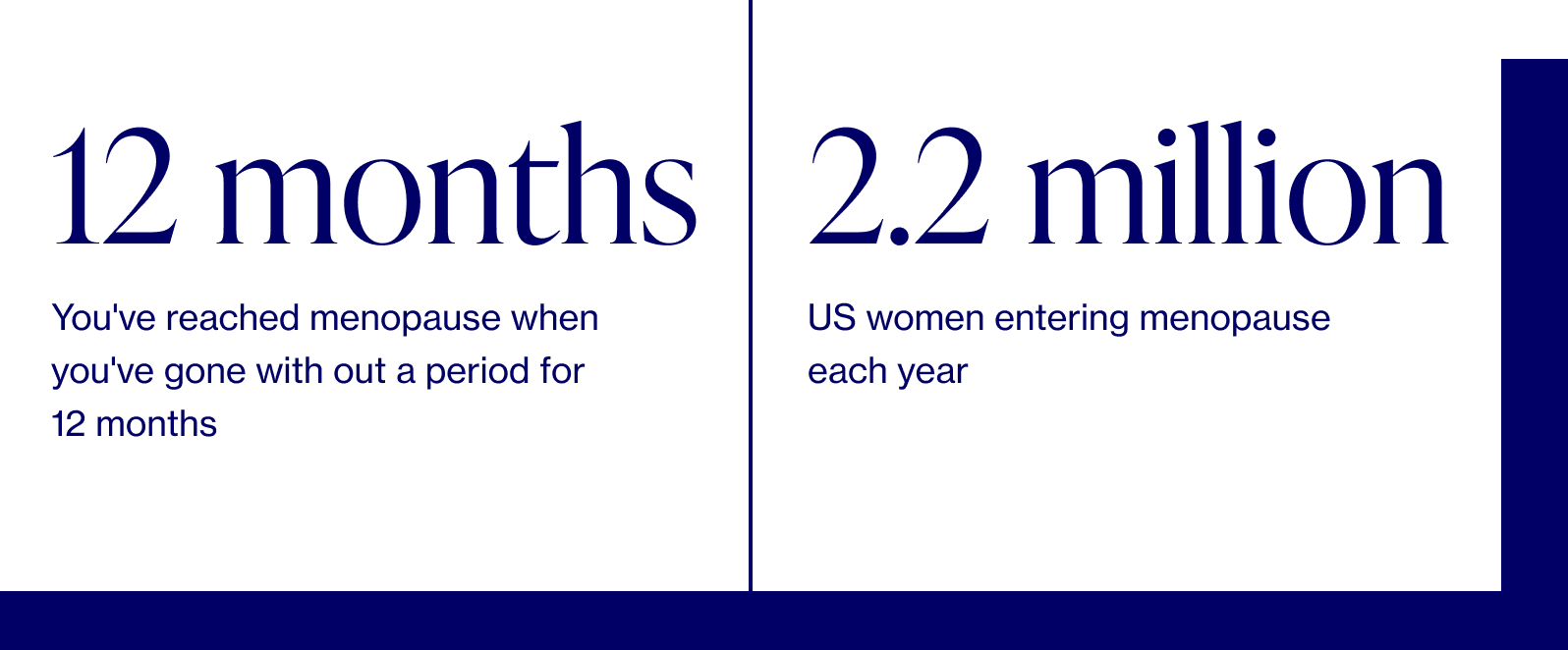
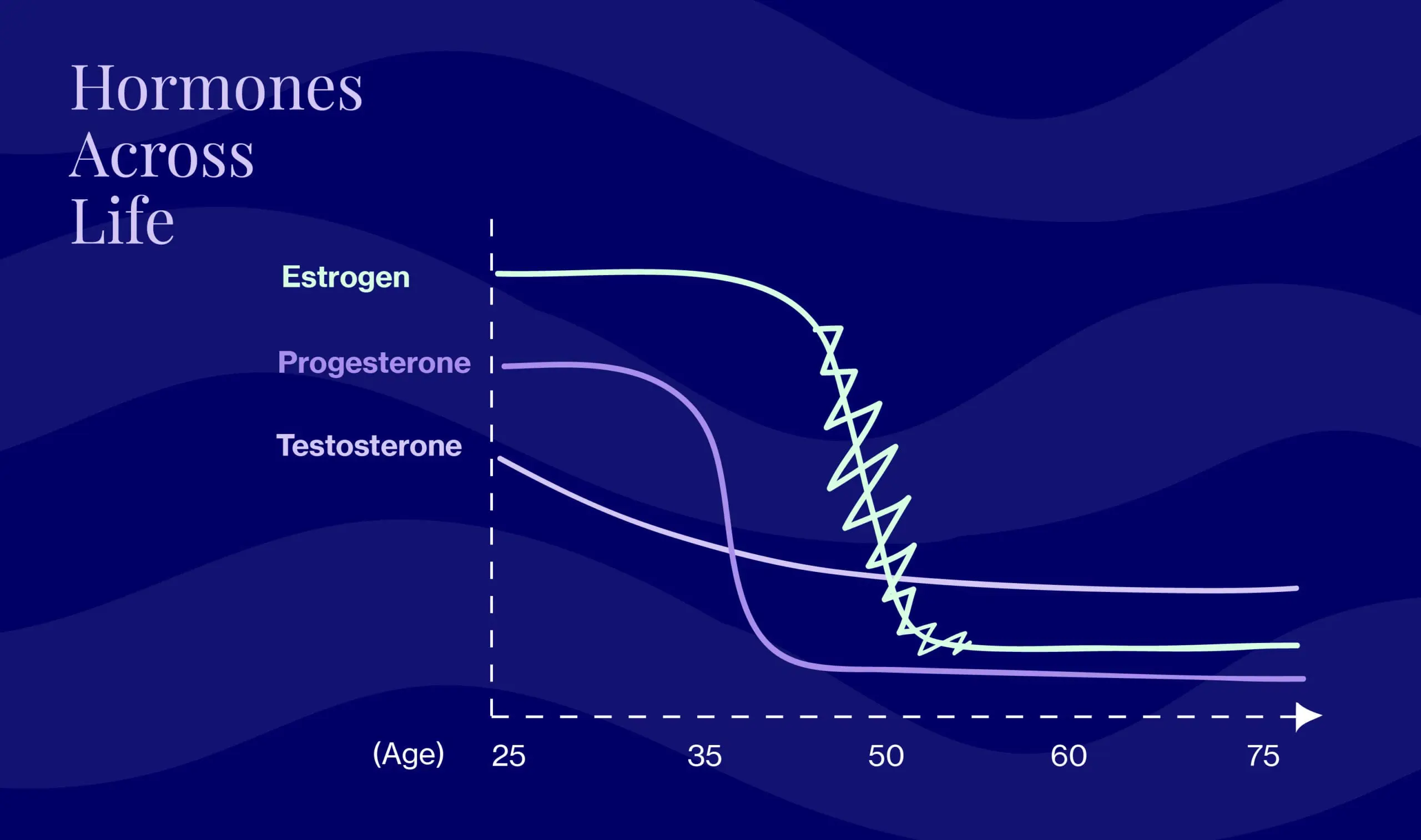
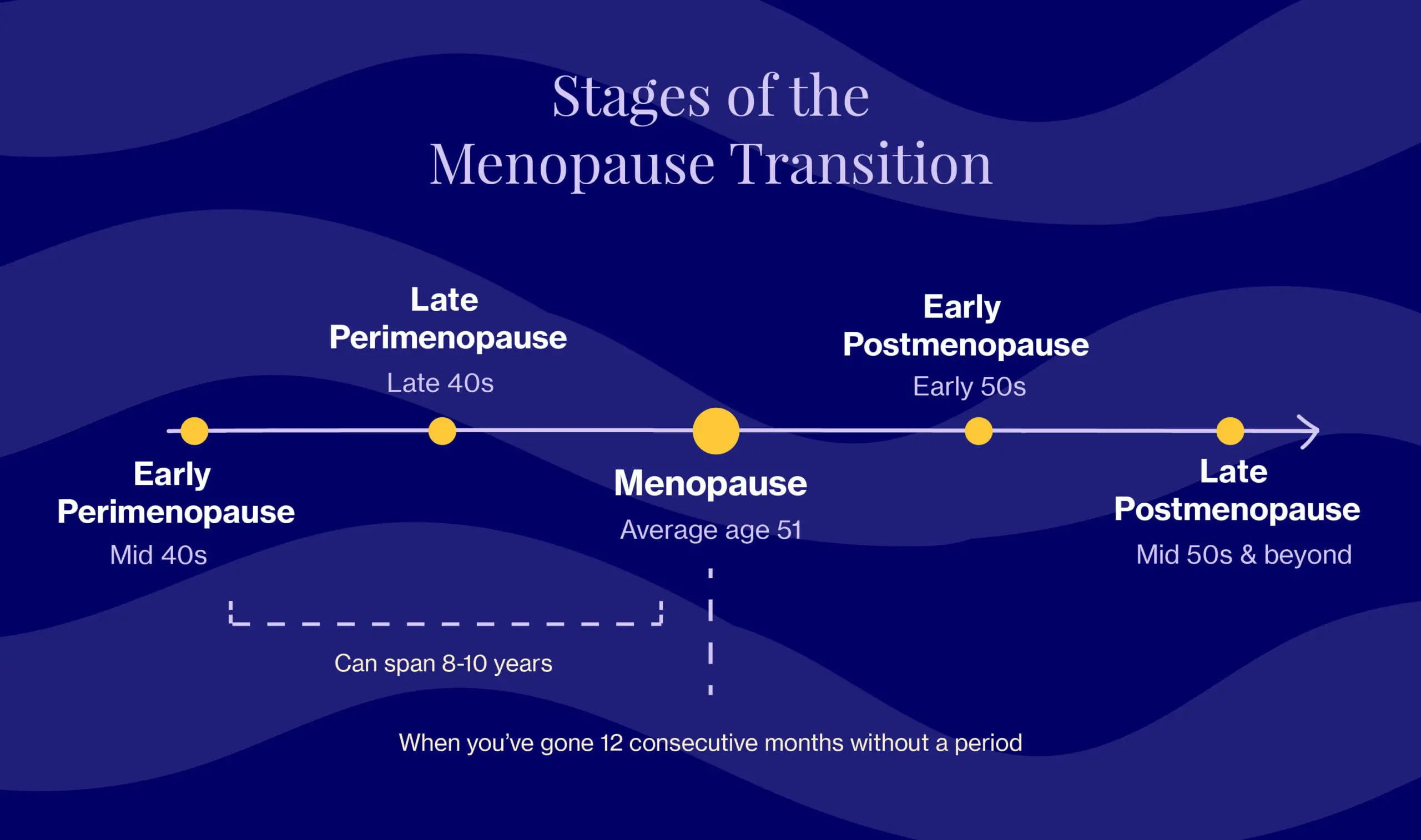
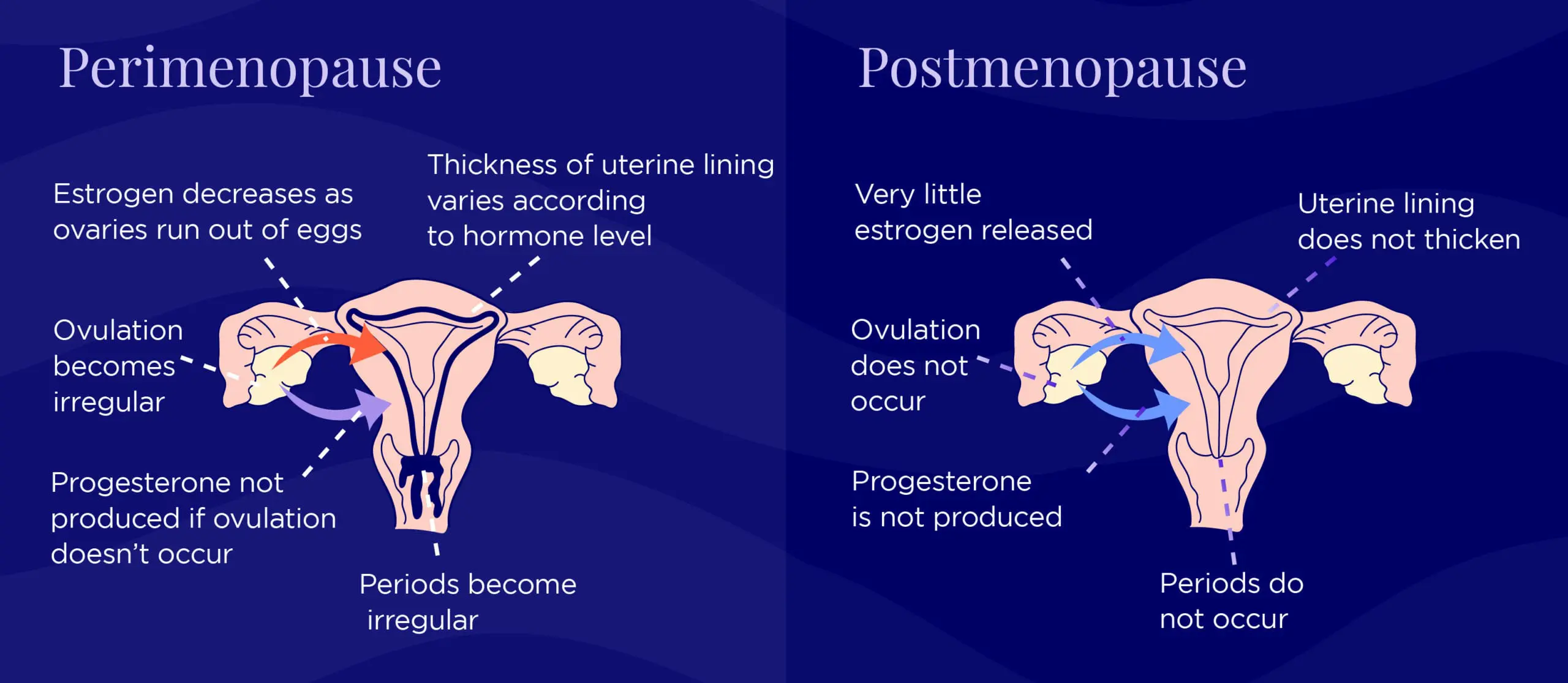
During the menopausal transition, the body’s production of two key female hormones, estrogen and progesterone, begins to progressively decline until you hit menopause which, officially speaking, occurs once you’ve gone 12 consecutive months without a period. Progesterone starts to decline first, and the decline is steep. Estrogen follows the same course but fluctuates a lot as it decreases (picture a roller coaster). Testosterone also declines on a gradual slope.
In Western societies, the average age is ~51, but many women start experiencing symptoms — like irregular periods and hot flashes — upwards of 8-10 years beforehand, during a stage known as perimenopause (aka “around menopause”). Once you’ve hit menopause, ovaries stop releasing eggs and cease production of the hormone, estrogen. You’ll remain here for the rest of your life, an era that’s also described as “postmenopause.”
Many of us assume menopause means we’re destined to feel tired, deflated, and, well, “meh” for years on end, which is simply not the case.
“So many women I’ve talked to see menopause as an ending. But I’ve discovered this is your moment to reinvent yourself after years of focusing on the needs of everyone else. It’s your opportunity to get clear about what matters to you and then to pursue that with all of your energy, time, and talent.” Oprah Winfrey
Perimenopause & menopause symptoms: what to expect
In an ideal world, we’d be able to package the symptoms of perimenopause, menopause, and postmenopause into neat, well-organized boxes that are unpacked one at a time. Unfortunately, menopause isn’t one-size-fits-all, and as Elektra’s founding physician, Dr. Anna Barbieri, MD explains, every woman experiences the transition differently.
“The experience can vary from individual to individual as well as across ethnic and cultural groups and across different countries and regions of the world,” says Dr. Barbieri.
That said, research does point towards certain patterns and trends. For example, we know that the symptoms typically associated with menopause (there are roughly 34) are actually experienced by most women during late perimenopause, peaking during the last two years due to an accelerated drop in estrogen levels. Below are the most common:
- Hot flashes/night sweats
- Irregular periods
- Vaginal dryness & discomfort during sex
- Urinary urgency & incontinence
- Difficulty sleeping
- Emotional changes (e.g., irritability, mood changes, anxiety/depression)
- Dry skin, eyes, or mouth
Post-Menopause
After you hit the menopause mark, you officially enter post-menopause. And remember, this is 12 months without a period. Many women will go 8-9-10 months and think they are in the clear, and then BAM, they get a period. And the clock starts over. Frustrating, to say the least.
Once you are post-menopausal, many symptoms tend to subside (hooray!) but some may persist, like vaginal and urinary symptoms (not hooray – but the good news is these can be addressed relatively easily!).
And, unfortunately, there are some longer-term health implications that come with being post-menopausal. We’re subject to increased risk of developing heart disease, diabetes, and osteoporosis.
The menopause transition is therefore THE time to take action every day to help prevent those conditions through self-care, healthy habits, and making sure we’re proactively getting the healthcare we deserve at this point in our lives.
What you can do
We’re all about equipping you with the know-how to understand your symptoms, and we especially emphasize the specific, tangible ways to manage them. Our goal is to empower YOU to take charge of your menopause journey, starting today.

Dr. Anna Barbieri, MD
Pro tip #2
Start a trigger journal! Review the list of symptoms and assess if you’re experiencing them on a scale of 1-10. Note triggers such as people, places, food, and sounds — you might be surprised by the patterns that emerge. This will help immensely when it comes to prep for a doctor’s visit, since you can refer back and give specific examples.
Pro tip #3
While most of us are aware of the physical symptoms of menopause like hot flashes, mood swings, and irregular periods, there are other less-well-known symptoms that affect brain, heart, and bone health. Estrogen protects each of these important body parts, so it’s important to build a routine that nourishes them through diet and strength training. Here’s a quick (but effective!) five-minute total body workout to get you started on strengthening your mind AND muscles.
A quick note about product recommendations…Elektra Health is not paid to feature any products. We just like them and think you might too, though we can’t guarantee any results.
Unless we go through “sudden” or premature menopause for medical reasons, we’ll spend a third or more of our lives in postmenopause. (The most common medical reasons include an oophorectomy, removal of the ovaries, and cancer treatments, among others.) This is a long time, so it’s important to understand what treatments are out there. Sure, some symptoms may be unavoidable, but there are still ways to have agency and manage the impact they have on your life. It’s all about optimizing your health for the long term.
Lifestyle
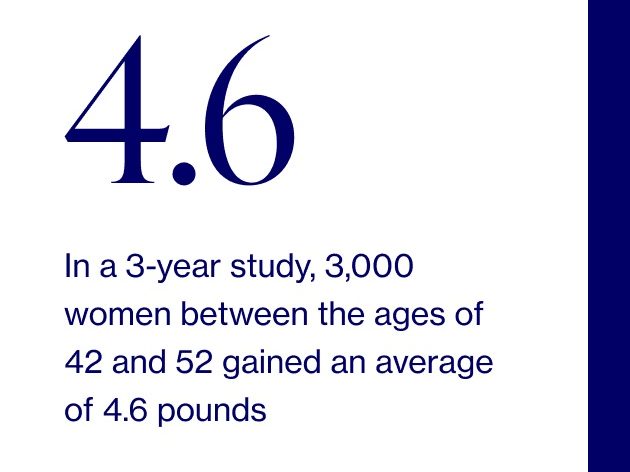
Lifestyle changes are paramount to temper the symptoms of menopause and postmenopause, whether or not you’re considering additional treatments, like hormone replacement therapy. Fortunately, research shows they can be as effective as medication, sometimes even eliminating the need for it. And the good news is that it doesn’t matter if you’re just starting perimenopause, beginning full-fledged menopause, or enjoying what many regard as the period-free liberation of postmenopause.
Leaning into healthy lifestyle changes at any age can greatly improve your symptoms, energy levels, and overall health. In other news, it's never too early and it's never too late.
“Hormones are very much affected by your mood, stress levels, sleep, exercise, and nutrition,” says Dr. Eva Selhub, MD, a physician, author, and resiliency expert — so much so, in fact, that studies have shown that a diet high in whole foods, especially vegetables is inversely correlated with menopause symptoms.
We also recommend building a “menopause support team.” Start by reviewing the list of symptoms, recording your experience with each on a scale of 1-10 (least disruptive to most disruptive), and prioritizing which to tackle first. Bring this list to your next doctor’s appointment and discuss with your doctor (if you don’t feel like your doctor is listening to you, then find a new doctor!). Having a doctor on your team who knows menopause is important. Elektra is ready to help and you can email [email protected] for help finding a local option.
In addition to your medical team, you need your personal cheerleaders. We encourage you to reach out to your confidants for support. Whether you just need someone to talk to or are looking for more concrete help (i.e. someone who’s at the ready if, say, sudden hot flashes make you want to stick your head in the freezer), start the conversation: I’m experiencing some symptoms, I think it’s perimenopause, and I need some support to get through this. We know there is still stigma and misunderstanding around the topic of menopause (hence Elektra Health!), but you owe it to yourself to not to experience this alone. And if one of your confidants is a woman in her mid-late 40s, she will likely have many of the same questions as you!
At any given moment, 50 million or more women in the U.S. are experiencing menopause, and a whopping 16% never discuss it with anyone at all. That needs to change!
In addition to building a “menopause support team,” consider meditation and mindfulness for stress management and other psychological symptoms associated with menopause. “These techniques,” explains Dr. Selhub, “…allow one to manage them better without distress.”
Alongside nutrition, physical activity, sleep, and mind-body interventions, there are a number of botanical and supplement solutions that can help, including soy isoflavones, black cohosh, and vitamin B6. Like hormone replacement therapy, however, some come with risks, side effects, and medication interactions, so it’s important to carefully evaluate your options and consult your healthcare provider (or Elektra!) first.
Menopause treatments
One of the most effective therapies for menopause is hormone replacement therapy (HRT), which involves taking a supplemental form of either estrogen — or estrogen and progestogen — to balance out the two and replace what the body is no longer naturally producing.
As with all medications, there are benefits and risks. For HRT, the benefits can include improving hot flashes, night sweats, sleep, mood, sex drive, and bone density, among others. If you’re thinking…but wait, doesn’t HRT cause breast cancer?…you’re not alone. Despite the fact that today, the Menopause Society (MS) considers HRT to be safe and effective for most women in menopause (especially when started prior to age 60 or within 10 years of menopause), it is still a hotly debated and often misunderstood topic. When factors such as health history and medical conditions, as well as the type, dose, and duration of therapy are considered, benefits of HRT can outweigh the risks.
Remember that there are also non-hormonal prescription options, including certain antidepressants, that can be used for severe symptoms, especially for women who cannot or do not wish to try hormonal therapies.
The bottom line? Yes, menopause comes with symptoms. No, you’re not alone in what you’re experiencing. Medications and supplements can play an important role, but don’t underestimate the power of nutrition, exercise, quality sleep, and stress management.
Reframing HOW you think about menopause is also incredibly powerful. For example, you can turn this time into an opportunity to step back, renew your identity, and set future goals.
Many of us will be retired and/or empty nesters with more time on our hands — perfect for considering what pursuits we used to love that we’ve not had time for lately Or, what new interests do you want to dive into? Not only will challenging ourselves in new ways keep our brain healthy, but it’ll also help us combat stress, stay present, and pursue long-overdue passions.
Remember, it’s totally within our power to tackle menopause with the same badass strength and perseverance that we’ve used to overcome everything else that’s come our way beforehand.
Ready? We are, too.
Disclaimer: This information is for general educational purposes, and should not be used as a substitute for medical advice, diagnosis, or treatment of any health condition or problem.
As with anything you put into your body, taking dietary supplements can also involve health risks. You should consult a medical professional before taking supplements and inform your doctor about any supplements, as well as any medications you already take, since there may be interactions.

